DR WARD DEAN ANSWERS YOUR QUESTIONS
We are delighted that Ward Dean, M.D., one of the world’s foremost antiaging physicians, has agreed to answer our readers’ questions.
Disclaimer: All educational information is offered under IAS terms and conditions. This information does not replace the advice of your physician and restrictions may apply in some countries. The opinions expressed by the writers may not be those of IAS.
Hi, my sister forwarded me this information and I have never heard of this breakthrough information.
What would be best for me? I was in the hospital last June for extreme high blood pressure.
They wanted to give me high blood pressure medicine and valium to to my anxiety and hypertension.
They said my heart was basically in layman’s terms been beating too hard and was becoming ‘beefy’ and that it was not relaxing well.
I am not sure what that means but I do have some ringing in my ears most of the time. I had no blockages and just a small amount of cholesterol in my neck.
I am looking at your site now and was looking at Ventfort and Chelohart.
I take a ton of vitamins including magnesium, and am on bioidentical hormone pellet inserted in hip. With progesterone subscrption, DIM and also Thyroid supplement. I have been thinking of not getting the pellet again and trying something natural for progesterone/estrogen/testosterone as the only reason I did the hormones was I thought it might help my blood pressure. My testosterone did not even register after blood test and estrogen was very low. Now they are in normal ranges. I am 57 years old.
I would appreciate any guidance very much. Thank you.
First, I agree with your decision to NOT repeat the pellet. Pellets produce unphysiologic long-term elevations of your hormones. Virtually all hormones have daily “diurnal” cycles. Hormones act on receptors. When hormone levels are high, receptor number and receptor sensitivity declines. Consequently, when hormone levels are chronically high, receptor sensitivity and receptor number is decreased. Consequently, the hormones become less effective.
Ringing in your ears could certainly be due to hypertension.
I recommend increasing your magnesium dosage to “bowel tolerance” (you cannot OD on magnesium, because it will give you diarrhea) and adding a teaspoon or two of “Light Salt” (which contains high potassium levels) to your diet.
If your blood pressure remains high, and your pulse rate is higher than the low 80s, I suggest a 3rd-generation beta blocker medication like carvedilol (“Co-Reg”) or nebevilol (“Bystolic”).
To elevate your testosterone, I suggest DHEA, 25 mg in the morning. DHEA is very efficiently converted to testosterone by most women. DHEA drops progressively with age, and is very important to maintain youthful levels of DHEA. It is not necessary to replace testosterone in women—this can be done with an appropriate dose of DHEA. Pregnenolone, 25 mg should also be considered in the morning. Pregnenolone converts preferentially to progesterone.
Rather than the long-acting pellets, I recommend bio-identical topical estrogen formulations such as IAS’s Esnatri, applied once per day.
With regard to the Russian bio-peptides, I suggest a combination of Pineal (Endoluten), Heart (Cheloheart) and Blood Vessel (Ventfort) peptides. Of course, these are slow-acting tissue/organ normalizers, so it is important to start with the more rapidly-acting pharmaceuticals, from which you should be able to wean yourself as the peptides take effect.
Ward Dean, MD
I run a small private clinic dealing mostly with cancer and auto-immune cases.
My question is, can I use peptide regulators for cancer, eg. the marrow peptide for multiple myeloma/Leukemia? It seems to me, that the marrow peptide could have some application for this use. Is there a tech resource or scientist/Doctor on your team that may be able to answer this question?
Regards,
That’s a very good idea. Leukemia, multiple myeloma, and other hematopoietic cancers are difficult to treat.
Some of the things I use for them are beta glucan,1 cyclodextrin,2 and honokiol (magnolia extract).3-6 I also suggest eating avocados!7
Although I have not yet used the biopeptides for leukemia or multiple myeloma, I agree with your thought to try them, as well. The biopeptides normalize the functioning of organs and tissues, and are without any known adverse effects.
Based on your insightful suggestion, I am going to incorporate the bone marrow (Bonomarlot) and pineal (Endoluten) peptides in my recommendations for my patients with leukemia, multiple myeloma, or myelodysplasia.
Ward Dean, MD
1. Weitberg, AB. A phase I/II trial of beta-(1,3)/(1,6) D-glucan in the treatment of patients with advanced malignancies receiving chemotherapy. J Exp Clin Cancer Res. 2008; 27(1): 40. doi: 10.1186/1756-9966-27-40
2. Yokoo, M, et al. 2-Hydroxypropyl-β-Cyclodextrin Acts as a Novel Anticancer Agent. PLoS One. 2015; 10(11): e0141946. doi: 10.1371/journal.pone.0141946
3. Battle TE, Arbiser J, Frank DA. The natural product honokiol induces caspase-dependent apoptosis in B-cell chronic lymphocytic leukemia (B-CLL) cells. Blood. 2005;106:690–7. [PubMed]
4. Hibasami H, Achiwa Y, Katsuzaki H, Imai K, Yoshioka K, Nakanishi K, et al. Honokiol induces apoptosis in human lymphoid leukemia Molt 4B cells. Int J Mol Med. 1998;2:671–3. [PubMed]
5. Marin GH, Mansilla E. Apoptosis induced by Magnolia Grandi fl ora extract in chlorambucil-resistant B-chronic lymphocytic leukemia cells. J Cancer Res Ther. 2010;6:463–5. [PubMed]
6. Ishitsuka K, Hideshima T, Hamasaki M, Raje N, Kumar S, Hideshima H, et al. Honokiol overcomes conventional drug resistance in human multiple myeloma by induction of caspase-dependent and -independent apoptosis. Blood. 2005;106:1794–800. [PMC free article] [PubMed]
7. Lee EA, et al. Targeting Mitochondria with Avocatin B Induces Selective Leukemia Cell Death. Cancer Res June 14 2015 75 (12) 2478-2488; DOI:10.1158/0008-5472.CAN-14-2676
I am 59 years old, born in India and living in Lithuania. My body can not handle being so far north. I guess this is because my neuroendocrine system does not funtion well in this weak sunlight. To relieve this each day I take:
St john‘s wort – 600 mg
Pregnenolone – 62.5 mg
DHEA – 20 mg.
Juvenon
Some vitamins and minerals
Probiotics
Omega 3 oil
Co Q 10
Digestive enzymes
I have taken DHEA and pregnenolone for years without any problems. My testosterone level has been normal – recent one was – 25.57 nmol / l, and the normal range is 5 to 20 nmol /l.
I began taking Endoluten 4 days ago. At first I felt better – but when I exercise, I feel sweaty very fast and my heart seems to be overloaded. Also, I am more constipated and I notice more hair falling out.
Is it possible that endoluten has some bad interaction with something I am taking, like DHEA or Pregnenolone?
I am thinking about starting endoluten again with just one capsule and take no DHEA, and cut down pregnenolone to 25 mg. Will that be a better balance ?
An IAS staffer mentioned that I consult my physician about Melatonin, in addition to the Endoluten (pineal polypeptide extract). I live in a place that is quite dark and believe my system makes enough melatonin. Do you think I should take some extra still ?
October 15th I started to take endoluten – 1 cap per day. And then I did not take any pregnenolone and DHEA. Also, I did not take any saw palmetto as it generates testosterone. Wanted to take no hormone- producing agents.
Then two weeks ago – I also added 1 cap cerluten (brain Biopeptide) and two caps glandokort (adrenal Biopeptide), plus alpha lipoic acid 150 mg per day and 160 mg of saw palmetto berry.
Do you think I should try this plan for 1 more month? Here the winter is dark in Lithuanina. And this plan is helping me here very much. And without pregnenolone and DHEA I can be here – this is amazing.
I have now taken 60 caps endoluten. As I follow the above plan – I will be taking 90 caps continously. Is this OK ?
After 1 month I will stop and take a break. And see how it continues to help me.
First, I don’t think Endoluten has anything to do with your feeling sweaty, having a rapid heart beat, being constipated, and your hair falling out. A characteristic of the biopeptides is their complete absence of adverse effects. They act to normalize the function of their respective organs and tissues.
Excess pregnenolone has been known to trigger cardiac arrhythmias, however, so you may benefit by a lower dose. I agree that you may do better by reducing your pregnenolone dose to about 25 mg in the morning. Your dose of DHEA, on the other hand, is quite low for a man your age. I suggest increasing DHEA to 50 mg in the morning.
I believe the IAS staffer who recommended Melatonin gave you good advice. You said that you “live in a place that is quite dark, and believe my system makes enough melatonin.”
However, dark environments result in chronobiological desynchronization, which may be the cause of most of your dysfunctional symptoms.1 I suggest 3-10 mg melatonin on an empty stomach, at bedtime each night. Dr. Pierpaoli’s special formulation of timed-release Melatonin-Se may be appropriate. Also, you may benefit by several sessions of “light therapy” for several hours each day.
You discontinued saw palmetto, under the erroneous impression that saw palmetto generates testosterone. However, the mechansim of Saw Palmetto is to block the conversion of testosterone to di-hydrotestosterone. Di-hydrotestosterone kills hair follicles–which results in hair loss–and stimulates prostatic hypertrophy. So I think it is a good idea to continue Saw Palmetto.
With regard to endluten—it is not recommended to take it for 90 days continuously. The usual recommendation is to take one capsule twice daily for 10-20 days, and then take a break for several months, repeating the cycle periodically, based on your response.
Overall, I think you’re on a pretty good program, which should help you to cope better with the relatively “polar climate” of Lithuania, compared to the one in which you grew up.
Ward Dean, MD
Reference:
1. Arendt, J. Biological Rhythms During Residence in Polar Regions. Chronobiol Int. 2012 May; 29(4): 379–394. doi: 10.3109/07420528.2012.668997
Dear Dr. Dean,
I have been following your original books since they came out, read and reread them along with Durk and Sandy. I still have them – Bibles… What a gift to be able to write to you.
I am 71 next month, and had Grave’s/RIA in 1986, age 40, the most devastating thing that has ever happened to me. I’ve been taking Armour Thyroid 120mg exclusively, except for trying others now and then, Losartan 50 mg for a couple of years, and Zelapar (selegiline/deprenyl) over 10 years as an Alzheimer’s preventive. I watched my great grandmother, grandmother, and mother succumb to Alzheimer’s, and always figured I could be next in line.
I have taken 1 and a half mg of Zelapar for ten years as a prophylactic, and would like to know what you think about changing to selegiline HCl instead? Zelapar is prohibitively expensive. What would be the equivalent HCl? I would rather take liquid deprenyl if I could find it by prescription, because my prescriptions are paid for. In the last year, I had both hips replaced from congenital disease, and have just done eye decompressions with diplopia and restoration surgery to go.
I have now done my genome and it is the most incredible paradigm shift by far, among many, for me. It is the key that has pulled everything together for diet, epigenetics, drugs, just everything!!! I have my life back with new attention.
Alzheimer’s is at the top of my Elevated Risk according to my genomic profile. My wonderful doctor said taking Zelapar at all is a maybe, and that it’s not such a high risk. I don’t otherwise need MOA-A or B inhibitors, I’m not good with the mesylates (Hydergine/Hydra-Pro), and am allergic to opioids and analgesics.
I would be so grateful for your opinion and any other drugs that might be more appropriate.
I am so clear and awake now, a true gift after losing the heart of my life.
Thanks for the kind words.
Yes, I agree that Zelapar is very overpriced. I don’t know how they’re getting away with it.
The marketing hype that the manufacturer of Zelapar uses to promote its use (“orally disintegrating tablets” versus the much less expensive “swallowed selegiline”) is a bunch of baloney.
The pharmaceutical manufacturer of Zelopar claims that the swallowed forms of selegiline (tablets and capsules) place one at risk for the so-called “cheese reaction” hypertensive crisis. However, this only occurs with unselective monoamine oxidase inhibitors. At the low doses of selegiline used by most patients and consumers (less than 10 mg per day), selegiline is a highly selective monoamine oxidase B (MAO-B) inhibitor that does not cause the cheese reaction. Consequently, you can safely and beneficially take the much more affordable (and equally effective) forms of deprenyl (Dep-Pro by IAS, or prescription selegiline HCl).
Prof. Josef Knoll, the principal developer of deprenyl, demonstrated in his later work that deprenyl has enhancing qualities in femto-picomolar concentrations, which leave MAO-B activity unchanged. He concluded that this previously unknown ‘enhancer effect’ is responsible for the unique therapeutic benefits of deprenyl.1
For Alzheimer’s disease (prevention and treatment), I’ve found that the world’s oldest synthetic drug, methylene blue2 is the most effective treatment there is. Methylene blue in daily doses of 100-150 mg per day3 really seems to “turn the lights on,” and causes those with significant degrees of dementia to become restored to normal or near-normal functioning. Methylene blue is available by prescription from compounding pharmacists, and reagent grade methylene blue can be obtained from many reputable chemical supply houses. Hopefully, IAS may be influenced to carry Methylene Blue, in the future.
The only adverse effect of methylene blue is that it causes shockingly blue urine. Consequently, I advise my methylene blue-consuming patients to stock up on blue underwear.
Ward Dean, MD
1. Miklya I. [Slowing the age-induced decline of brain function with prophylactic use of (-)-deprenyl (Selegiline, Jumex). Current international view and conclusions 25 years after the Knoll’s proposal]. [Article in Hungarian] Neuropsychopharmacol Hung. 2009 Dec;11(4):217-25.
2. Schirmer RH1, Adler H, Pickhardt M, Mandelkow E. “Lest we forget you–methylene blue…”. Neurobiol Aging. 2011 Dec;32(12):2325.e7-16. doi: 10.1016/j.neurobiolaging.2010.12.012.
3. Wischik CM, Staff RT, Wischik DJ, Bentham P, Murray AD, Storey JM, Kook KA, Harrington CR. Tau aggregation inhibitor therapy: an exploratory phase 2 study in mild or moderate Alzheimer’s disease.J Alzheimers Dis. 2015 Jan 1;44(2):705-20.
Dr. Dean,
I am a very active 25-year-old, but I am afraid that my testosterone levels are not where they should be. My libido is low and I have very limited sex drive, which I find is odd for a guy my age and as active as I am.
That being said, I did suffer a major head injury a few years back and it seems to be shorty there after that my issues began to rise. I have done limited reading on head trauma and how it can lead to hormones being off in the body. Thanks for help in advance.
Matt
Hi, Matt,
It is not uncommon for those who have suffered a traumatic brain injury (TBI) to develop post-injury endocrine changes.1, 2 These are believed to result from damage to the hypothalamus and/or pituitary as a result of the trauma. Have you had your hormone levels tested? That is logically an early step to take. Also, did you obtain/retain any hospital records or diagnostic tests from the injury?
My recommendation is to first obtain a comprehensive endocrine panel, which will enable a hormone replacement program to be developed. If significant neuroendocrine abnormalities are found, in addition to appropriate hormone replacement therapy, I also recommend that you consider supplementation with a regimen of Russian bio-peptides.
The Russian peptide bio-regulators stem from the research that was begun in the late 1970s, initated by Prof. Vladimir Dilman and his research team.3 Although Prof. Dilman passed away prematurely in 1994, his work has been carried on by his students/associates, Profs. Vladimir Anisimov and Vladimir Khavinson (it is curious that the premier scientists in this field all seemed to be named Vladimir). Phil Micans, editor and publisher of the journal Aging Matters (www.antiaging-systems.com) conducted a recent interview with Prof. Khavinson, reviewing the history, mechanisms, and current research with the ever-growing body of available peptides.4
The peptide bio-regulators are taken in cycles, usually twice daily for 10-20 days, and repeated every 2-3 months until the desired results are achieved. The objective is to restore function of tissues to more youthful levels. In your case, presuming that disruption of your hypothalamo-pituitary-testicular axis is found, I would recommend a combination of pineal (Endoluten), brain (Cerluten), and testicular (Testoluten) peptides. With an appropriate regimen, hormone replacement therapy can often be discontinued, as the body’s tissues restore their normal function.
Let me know if you have any further questions,
Ward Dean, MD
References:
1. Kopczak A, Krewer C, Schneider M, Kreitschmann-Andermahr I, Schneider HJ, Stalla GK.
The Development of Neuroendocrine Disturbances over Time: Longitudinal Findings in Patients after Traumatic Brain Injury and Subarachnoid Hemorrhage. Int J Mol Sci. 2015 Dec 22;17(1).
2. Izzo G, Tirelli A, Angrisani E, Cannaviello G, Cannaviello L, Puzziello A, Vatrella A, Vitale M. Pituitary dysfunction and its association with quality of life in traumatic brain injury. Int J Surg. 2016 Apr;28 Suppl 1:S103-8.
3. Dilman VM. [Improvement of the indicators of cellular immunity under the effect of polypeptide epiphyseal extract (epithalamine)]. Vopr Onkol. 1977;23(6):7-9.
4. Micans, P. The new Russian peptide revolution. Aging Matters, 25th Anniversary Edition 2016, pp. 6-9.
Dear Dr. Dean, I want to try Goat’s Rue for my diabetic mother, but is it safe long-term? I found this:
ww.ebmconsult.com/articles/Goats-rue-french-lilac-diabetes?from=pw
DP
Dear Mr. DP,
I think you may have pretty well answered your own question, as indicated in several of the references that you kindly provided in the attached article. The active ingredient in goat’s rue (gallega oficinalis) is guanidine. As the article you sent summarized, “While guanidine-containing supplements have glucose-lowering properties, the toxicity profile outweighs any potential benefits provided and should not generally be used or recommended.”
Phenformin was a previously-available pharmaceutical derivative of goat’s rue which was removed from the US market in the late 1970s due to excess deaths from lactic acidosis. It was not until the mid-90s that another biguanide, Metformin, was introduced in the US. Metformin is much safer than phenformin, and has much less tendency (if any) to cause lactic acidosis (although lactic acidosis is still listed as an adverse effect of Metformin in the product literature). Metformin has been used with an excellent safety record for over 75 years (it’s been available in Europe since the 1950s). In the Diabetes Prevention Program Research Group’s study, over 18,000 patient-years of follow-up has accrued, with about 20% of the cohort now 70 or older. There have been no cases of lactic acidosis or significant hypoglycemia.(1)
I’ve used both goat’s rue and metformin in my patients. Metformin is cheaper, safer and far more effective than goat’s rue. This is one drug that is superior to its herbal prototype. For once, the pharmaceutical companies got it right! Despite the erroneous beliefs of many physicians, Metformin is neither nephrotoxic nor hepatotoxic, and can be safely used even in those with severely impaired kidney and liver function. Just titrate the dose down to whatever fractional dose the patient can tolerate, however. I had a diabetic patient who came to me on insulin, with a GFR (glomerular filtration rate) of 15! His nephrologist was recommending dialysis. After discontinuing insulin, and initiating a very low dose of metformin, his GFR began to improve, his other labs got better, and his nephrologist took him off the “critical list.”
I would not waste time fooling with goat’s rue, and recommend your mother include Metformin in her regimen.
Ward Dean, MD
1. The Diabetes Prevention Program Research Group. Long-Term Safety, Tolerability, and Weight Loss Associated with Metformin in the Diabetes Prevention Program Outcomes Study. Diabetes Care 2012 Apr; 35(4): 731-737.
Dr Dean
I did an Adrenal Stress Profile saliva test and my Cortisol to DHEA ratio is 8.67 which is very high, all my cortisol levels were low with a Sum of 22.1 nM/L and the DHEA-S was 2.55ng/mL which is also low. I’ve started taking Glandokort®, vitamin C and B5, 12.5 mg DHEA and pregnenolone, also taking an Adrenal Support which has 5mg hydrocortisone with B5 and vitamin C in it. Taking 5mg -15mg daily of that.
My main problem has been short term memory loss with brain fog as I’m a Respiratory Therapist who works in the ICUs running the ventilators. As of now I haven’t been working due to this problem, as its truly too unsafe to be working. My question is, is there anything else I should be taking and how long should I take the Glandokort?
Thanks for any help as I need to get well and back to work saving lives.
D.R.
Hi, D.R.,
The dose of DHEA replacement you are taking is pitifully low for most males. I usually start with 50 mg per day, taken first thing in the morning. Women, of course, must be more judicious, due to their very efficiently converting DHEA into testosterone, which is the limiting factor for most women. I think you’ll do better with a higher dose.
With regard to the Glandokort®, I recommend 1 capsule twice daily for 10-20 days, repeating the dose in a cycle about every three months. That’s the advantage of the Russian Bio-Peptides, in that they are not required to be taken on a continuing, ongoing basis. They stimulate the body to restore the functioning of the tissue from which the peptides were derived. The Russians also recommend that the blood vessel polypeptide extract (Ventfort®) also be included in virtually every Bio-Peptide regimen, as it seems to really enhance the effect of the others.
The hydrocortisone you’re taking is in a pretty low dose, so it’s probably OK for the short term, but I’m sure you are aware of the problems with chronic use, in terms of further shutting down your body’s endogenous production of cortisol. I hope you’ll be able to wean yourself from the use of that hormone.
In addition, concerning your cortisol and cortisol/DHEA ratio, I’d suggest checking on your thyroid—it is a common cause of brain fog and muddled thinking. Look over the thyroid questionnaire I’ve attached, and see how many “yeses” you checked off. If you’ve checked more than 1/3, I suggest adding desiccated thyroid (ERFA or Nature-Throid) to your regimen. Begin with 1 grain in the morning, and gradually titrate the dose upward every month or so, until your brain fog and other symptoms clear, or you note palpitations, increased heart rate, or increased body temperature. The warning in the PDR regarding thyroid replacement therapy cautions practitioners to first address adrenal issues before starting thyroid replacement. In practice, that’s rarely done–but in your case, you’re ahead of the game.
If you’ve had your thyroid checked, and you were told it was “normal,” make sure that it was a comprehensive panel that included T3, free T3, Thyroid Peroxidase Antibodies (TPO), and anti-thyroglobulin antibodies. It’s amazing how often a case of Hashimoto’s thyroiditis is overlooked by physicians who only check TSH, and maybe T4. Dr. Pierpaoli recommends that TSH be pushed down to near-zero–and I find that in most cases, he’s right!
One other suggestion is to add Metformin to your regimen. Metformin is not just for diabetics, or for those with insulin resistance. Metformin is a “multi-hormone receptor sensitizer.” It does more than overcome insulin resistance. It also restores receptor sensitivity to estrogen, cortisol and other steroid hormones like progesterone and testosterone–and maybe even thyroid.
Give these suggestions a try, and let me know how you do–and when you are able to get back to work.Good luck,
Ward Dean, MD
Dr Dean
I did an Adrenal Stress Profile saliva test and my Cortisol to DHEA ratio is 8.67 which is very high, all my cortisol levels were low with a Sum of 22.1 nM/L and the DHEA-S was 2.55ng/mL which is also low. I’ve started taking Glandokort®, vitamin C and B5, 12.5 mg DHEA and pregnenolone, also taking an Adrenal Support which has 5mg hydrocortisone with B5 and vitamin C in it. Taking 5mg -15mg daily of that.
My main problem has been short term memory loss with brain fog as I’m a Respiratory Therapist who works in the ICUs running the ventilators. As of now I haven’t been working due to this problem, as its truly too unsafe to be working. My question is, is there anything else I should be taking and how long should I take the Glandokort?
Thanks for any help as I need to get well and back to work saving lives.
D.R.
Hi, D.R.,
The dose of DHEA replacement you are taking is pitifully low for most males. I usually start with 50 mg per day, taken first thing in the morning. Women, of course, must be more judicious, due to their very efficiently converting DHEA into testosterone, which is the limiting factor for most women. I think you’ll do better with a higher dose.
With regard to the Glandokort®, I recommend 1 capsule twice daily for 10-20 days, repeating the dose in a cycle about every three months. That’s the advantage of the Russian Bio-Peptides, in that they are not required to be taken on a continuing, ongoing basis. They stimulate the body to restore the functioning of the tissue from which the peptides were derived. The Russians also recommend that the blood vessel polypeptide extract (Ventfort®) also be included in virtually every Bio-Peptide regimen, as it seems to really enhance the effect of the others.
The hydrocortisone you’re taking is in a pretty low dose, so it’s probably OK for the short term, but I’m sure you are aware of the problems with chronic use, in terms of further shutting down your body’s endogenous production of cortisol. I hope you’ll be able to wean yourself from the use of that hormone.
In addition, concerning your cortisol and cortisol/DHEA ratio, I’d suggest checking on your thyroid—it is a common cause of brain fog and muddled thinking. Look over the thyroid questionnaire I’ve attached, and see how many “yeses” you checked off. If you’ve checked more than 1/3, I suggest adding desiccated thyroid (ERFA or Nature-Throid) to your regimen. Begin with 1 grain in the morning, and gradually titrate the dose upward every month or so, until your brain fog and other symptoms clear, or you note palpitations, increased heart rate, or increased body temperature. The warning in the PDR regarding thyroid replacement therapy cautions practitioners to first address adrenal issues before starting thyroid replacement. In practice, that’s rarely done–but in your case, you’re ahead of the game.
If you’ve had your thyroid checked, and you were told it was “normal,” make sure that it was a comprehensive panel that included T3, free T3, Thyroid Peroxidase Antibodies (TPO), and anti-thyroglobulin antibodies. It’s amazing how often a case of Hashimoto’s thyroiditis is overlooked by physicians who only check TSH, and maybe T4. Dr. Pierpaoli recommends that TSH be pushed down to near-zero–and I find that in most cases, he’s right!
One other suggestion is to add Metformin to your regimen. Metformin is not just for diabetics, or for those with insulin resistance. Metformin is a “multi-hormone receptor sensitizer.” It does more than overcome insulin resistance. It also restores receptor sensitivity to estrogen, cortisol and other steroid hormones like progesterone and testosterone–and maybe even thyroid.
Give these suggestions a try, and let me know how you do–and when you are able to get back to work.Good luck,
Ward Dean, MD
Symptoms of Hypothyroidism Questionnaire
Hypothyroidism is a condition of insufficient output from the thyroid gland. Broda Barnes, M.D., Ph.D., perhaps the most famous thyroid researcher and author of Hypothyroidism: The Unsuspected Illness, reports that the symptoms related to low thyroid vary widely and may include the following (please check all that apply):
____Sensitivity to cold – especially in hands and feet
____Fatigue–reduced energy levels
____Weight gain
____Inability to lose weight despite constant dieting
____Infections-especially respiratory infections
____Frequent bouts of cold or flu
____Asthma and allergies
____Decreased perspiration
____Dry, coarse, leathery skin; pale
____Poor circulation
____Coarse hair or hair loss
____Dry eyes/blurred vision
____Swelling or puffy eyelids
____Digestive problems, irritable bowel syndrome, or acid indigestion
____Constipation
____Headaches–moderate to severe
____Poor short term memory and concentration
____Arthritis, joint pains
____Low blood pressure
____High blood pressure
____High cholesterol or atherosclerosis
____Diabetes
____Hypoglycemia
____Low libido
____Anxiety/panic attacks
____Depression-moderate to severe
____Behavioral and emotional disorders
____Wounds that heal slowly
____Menstrual problems (include PMS or hysterectomy)
____Infertility
____Enlarged thyroid-goiter
____Acne
____Lateral halves of eyebrows missing
Dear Dr. Dean,
My elderly father has congestive heart failure and kidney problems. He currently is retaining fluid in his lower legs and feet. When he was hospitalized, they insist on IV diuretics. They are ineffective and do more damage to his kidneys. He feels better now on no medication. He currently is on Furosimide orally (40 mg twice/day) and Aldactone 12.5 mg twice/day–But he isn’t tolerating them well. Additionally, we have discovered they are counterintuitive. What would you recommend from your site, given that he is not able to take many pills? Liquids would be great.
Thank you,
L.T., USA
Hi, L.T.,
I could probably be more helpful, if I had a little more information, such as your dad’s age, his degree of kidney dysfunction (i.e., his GFR [glomerular filtration rate]), and what problems he is having with his medications?
As you have probably become aware, diuretics such as furosemide and aldactone are among the mainstays of treatment for congestive heart failure. This is to relieve the obvious “backing up” of accumulated fluid in the lower legs caused by the inability of the heart to propel the blood forward. If the condition is not alleviated, fluid further accumulates in the abdomen and lungs, causing shortness of breath or wheezing at night, when in a completely horizontal position. This causes those with CHF to require several pillows at night, or even need to sleep sitting up.
The maximum daily dose of furosemide (Lasix) is 600 mg/day, so 40 mg twice daily is not generally too much. In fact, I would consider boosting the dose to three times/day, and not use Aldactone (spiranalactone). Aldactone is a potassium-sparing diuretic. Instead, I would recommend that your dad consume about one teaspoon of Lite Salt each day, available in your grocery store. Lite Salt contains 230 mg sodium, and 340 mg potassium, per quarter teaspoon. Lasix will cause a significant amount of potassium to be excreted in the urine, which will be replaced with the Lite Salt.
For more details on the use of potassium to treat hypertension, I recommend Dr. Richard D. Moore’s book (available from Amazon)–The High Blood Pressure Solution: A Scientifically Proven Program for Preventing Strokes and Heart Disease. (I just provided you with the “meat” of the book in the preceding paragraph.)
Endothelial Dysfunction
Endothelial cells line all of the 60,000 or-so miles of our vascular system—arteries, arterioles, capillaries, venules, and veins. Virtually all diseases—especially those of the heart, vascular system, and kidneys—originate with endothelial dysfunction (Fig. 1). A biomarker of endothelial function is asymmetric dimethyl arginine (ASDMA).1 Ask your dad’s physician to check this biomarker.
A number of supplements and medications are able to reduce ASDMA. IAS’s product, NEO-40 is specifically designed to optimize endothelial function. Neo-40 contains a combination of beet root extract (the richest nutritional source of nitric oxide), plus the amino acid L-citrulline (which converts to arginine, in the Urea Cycle). The ratio of asymmetric dimethyl arginine to arginine is a key indicator of endothelial function.2 The lower the ASDMA, and the higher the arginine, the better the prognosis.
Other substances that will reduce ASDMA include N-Acetyl Cysteine,3 alpha lipoic acid,4 Metformin5 (note, however, that although Metformin is not nephrotoxic, since it is excreted through the kidneys, those with impaired kidney function must take a reduced dose of Metformin), and the anti-hypertensives Lisinopril6 and the third-generation beta-blockers nebivolol (Bystolic) or carvedilol (CoReg).7 Note that a second-generation beta-blocker, metoprolol, will actually increase ASDMA, worsening endothelial function.
For long-term improvement of cardiovascular and renal function, you might also consider several courses of the appropriate Russian bio-peptides. I recommend a combination of Pineal (Endoluten), Heart (Chelohart), Kidney (Pielotake), and Blood vessels (Ventforte).
If your dad has problems taking oral tablets or capsules, Neo-40 should not be a problem, as it dissolves sublingually. Other substances can either be dissolved in water or any other beverage, or even be taken rectally.
Ward Dean, MD
1. Sibal L, Agarwal SC, Home PD, and Boger RH. The Role of Asymmetric Dimethylarginine (ADMA) in Endothelial Dysfunction and Cardiovascular Disease. Curr Cardiol Rev. 2010 May; 6(2): 82–90. doi: 10.2174/157340310791162659
2. Notsu Y, Yano S, Shibata H, Nagai A, Nabika T. Plasma arginine/ADMA ratio is a sensitive risk marker for atherosclerosis. Atherosclerosis. 2015 Mar;239(1):61-6. doi: 10.1016/j.atherosclerosis.2014.12.030.
3. Thaha M, WidodoPW, Yogiantoro M, Tomino Y. Intravenous N-acetylcysteine during hemodialysis reduces asymmetric dimethylarginine level in end-stage renal disease patients.Clin Nephrol. 2008 Jan;69(1):24-32.
4. Mittermayer F, Pleiner J, Francesconi M, Wolzt M. Treatment with alpha-lipoic acid reduces asymmetric dimethylarginine in patients with type 2 diabetes mellitus.Transl Res. 2010 Jan;155(1):6-9. doi: 10.1016/j.trsl.2009.08.004.
5. AsagamiT, AbbasiF, StuelingerM, LamendolaC, McLaughlinT, CookeJP, ReavenGM,
TsaoPS. Metformin treatment lowers asymmetric dimethylarginine concentrations in patients with type 2 diabetes. Metabolism Clinical and Experimental, 2002, Volume 51, Issue 7, Pages 843–846
6. Chen JW, Hsu NW, Wu TC, Lin SJ, Chang MS. Long-term angiotensin-converting enzyme inhibition reduces plasma asymmetric dimethylarginine and improves endothelial nitric oxide bioavailability and coronary microvascular function in patients with syndrome X.Am J Cardiol. 2002 Nov 1;90(9):974-82.
7. Oğuz A, Uzunlulu M, Yorulmaz E, Yalçin Y, Hekim N, Fici F. Effect of nebivolol and metoprolol treatments on serum asymmetric dimethylarginine levels in hypertensive patients with type 2 diabetes mellitus.Anadolu Kardiyol Derg. 2007 Dec;7(4):383-7.
Dr. Dean,
I read with interest the article on Centrophenoxine in the recent Aging Matters magazine. The article suggests that the benefit of Centrophenoxine may be from its ability to remove lipofuscin, which DMAE can do and DMAE is half of the Centrophenoxine molecule. But the other half is PCPA (p–Chlorophenylalanine), which essentially sends brain serotonin levels down to next to nothing. That is a little worrisome and it has been the reason I never have recommended this supplement in my practice. I suppose someone with serotonin syndrome might really benefit from it, but I am concerned that the benefit of centrophenoxine is no better than DMAE, but the down side from the PCPA could be significant.
I understand your concern about PCPA—and your confusion. PCPA (as p-chlorophenylalanine) is indeed an inhibitor of the conversion of tryptophan to 5HTP, the rate-limiting step in serotonin biosynthesis. Doses of PCPA (as p-chlorophenylalanine) ranging from 1-4 gm per day can reduce synthesis of serotonin up to 88 percent.1 However, the PCPA half of centrophenoxine is not p-chlorophenylalanine. PCPA in Centrophenoxine stands for p-chlorophenoxyacetic acid—which confusingly uses the same abbreviation. Centrophenoxine actually increases brain serotonin in experimental animals, and presumably, in humans as well. Centrophenoxine given to rats caused a dose-dependent elevation of serotonin in three different brain regions, particularly in the brain stem. p-chlorophenoxyacetic acid, given separately, resulted in identical changes.2 Subsequent studies in Bulgaria confirmed these findings.3,4 In a double-blind study in 50 demented patients, treatment for 8 weeks with Centrophenoxine resulted in improved psychometric and behavioral performance in about 50% of the treated patients.5 Professor Imre Nagy reports that he and his staff have taken 500 mg/day of Centrophenoxine since 1976. Although he admits that this cannot be considered a scientific experiment, all the participants agree that they appear to be in better physical and mental health than their untreated peers in their family and community, and have had no adverse effects from this treatment for over 40 years.6 We’ll try to spell out the complete meaning of PCPA to avoid this confusion in the future.
References:
1. Engelman K, Lovenberg W, Sjoerdsma A. Inhibition of serotonin synthesis by para-chlorophenylalanine in patients with the carcinoid syndrome. New Eng J Med, 1967, 277(21) 1103-1108.
2. Koga T. [Increase of brain serotonin and its metabolite in rats caused by meclofenoxate].Nihon Yakurigaku Zasshi. 1976;72(4):392-402.
3. Petkov VV, Grahovska T, Petkov VD, Konstantinova E. Effects of meclofenoxate on the level and turnover of biogenic monoamines in the rat brain.Arzneimittelforschung. 1985;35(12):1778-81.
4. Petkov VD, Stancheva SL, Tocuschieva L, Petkov VV. Changes in brain biogenic monoamines induced by the nootropic drugs adafenoxate and meclofenoxate and by citicholine (experiments on rats).Gen Pharmacol. 1990;21(1):71-5.
5. Fulop T, Worum I, Csongor J, Leovey A, Szabo T, Pek G, and Zs.-Nagy I. Effects of centrophenoxine on body composition and some biochemical parameters of demented elderly people s revealed in a double-blind clinical trial. Arch Ger and Ger. 1990;10(3):239-252.
6. Zs.-Nagy I. Aging of cell membranes: Facts and Theories, In: Interdisc Top Gerontol. Basel, Karger. 2014, 39, 62-85.
Dr. Dean,
My doctor recently had me do a 6-hour urine provocation test using one IV bag of DMPS followed by one bag of EDTA.
The results showed that my mercury level is high, so she would like me to do 6 bags of DMPS over a 6-month period. In your opinion, how reliable is this method of testing?
I have read that it may not be an accurate way to measure heavy metals since pretty much anyone will show elevated levels of metals in their urine after being administered IV DMPS. If it is an accurate test, I have also read many reasons not to treat high mercury with IV DMPS and that oral DMSA may be a better option.
I had no noticeable side effects from the provocation test. Would IV DMPS be a good treatment plan for me, or should I stick with oral DMSA?
I appreciate any insight that you can provide.
Thank You,
J.L.
Dear J.L.,
I believe the urine chelation challenge test is the most accurate way to determine heavy metal toxicity. Virtually any amount of mercury or lead is toxic—and if, as you say, anyone will have heavy metals in their urine after DMPS or EDTA, then virtually everyone should undergo chelation therapy to eliminate these toxins. If there are no heavy metals in the body, they will not show up on these tests. But the more mercury or lead in your body, the greater the amounts that will show up in your urine following the chelation challenge.
IV DMPS and oral DMSA are both very effective chelators of mercury, and EDTA is somewhat less effective. The choice of which to use is really up to the physician and the patient. DMSA was formerly available in the U.S. as a dietary supplement, but was knocked off the market several years ago by the FDA (“If the FDA doesn’t like something, it’s got to be good”). Unfortunately, prescription DMSA (Succimeer) is quite expensive (the dietary supplement was very cheap). Oral DMSA, of course is very convenient, while the IV DMPS requires periodic visits to your physician’s office.
So the choice is really up to you. Both treatments will work—and if your mercury levels are up, I recommend that you select one treatment modality and get started.
Ward Dean, MD
Dear Dr. Dean
I just purchased your growth hormone releasing hormone called Serm Pro (sermorelin).
I have been taking high dose prednisone for almost five years and am trying to wean myself off of the medicine. I was having severe muscle pain in my lower back to the point that I could not take care of myself. I assume the problem was caused by my obesity. Ibuprofen was not helpful and prednisone was prescribed at 20mg, and it helped a lot, but when I tried to go off of it the side effects made it too difficult. Besides giving me pain all over my muscles, it made me so profoundly weak that my muscles would not even respond to my brain signals. I couldn’t even roll over in bed. I have taken over 100mg. per day for short periods of time. Although it’s difficult, I have been able to reduce my dosage many times, but then the side effects kick in so strongly that the only way to get enough strength to take care of myself is to increase my dosage to a much higher level. This has gone on for four and a half years.
Whenever I decrease my dose I get profoundly weak and in pain to the point of where I can’t take care of myself. The only advice doctors give me is to lower my dosage in small increments over a long period of time, but this has never worked for me. I am suffering many side effects from the Prednisone such as diabetes, thin skin to the point of where it tears, lymphedema, cellulitis, weakness and pain, and massive fluid retention. I have now lost the ability to walk.
In reading about the effects of growth hormone, they seem to be the opposite of Prednisone. So I bought your product called Serm-Pro. I am hoping that taking the Serm Pro at the same time I am reducing my dose of Prednisone will compensate for the negative effects that I experience as I reduce my dosage of Prednisone. Can you give me any advice as to whether you think this will help and also how much I should take and when, and how long I should take it before it reaches its full effectiveness and any other information that you think might be helpful.
Besides the prednisone, I take Norco for pain, Ativan for anxiety and Lasix for fluid retention. I also have developed diabetes because of the prednisone. My blood sugar levels are normal until I take the prednisone and then they rise. As for lab values, the only thing that doctors have treated is my low vitamin D levels. I have weak muscles and brittle bones and thin tearing skin, and massive fluid retention. I am 53 years old, 5 feet 10 inches tall, and weigh about 600 pounds.
In particular, do you sell any other products that I could take along with the Serm Pro that might also be helpful in my situation? I am very overweight both naturally and because of the Prednisone. Thank you,
Mr. B.A.
Dear Mr. B.A.,
I believe we have many issues to resolve, not just your dependence on prednisone. In addition to prednisone dependence, we need to address your morbid obesity, diabetes, probably osteoporosis, and sarcopenia.
First, I recommend testosterone cypionate, 200 mg intramuscularly every three weeks. The anabolic effects of testosterone will counteract the catabolic effects of prednisone, to some degree.
We also need to get serious about your obesity, which as you pointed out, may have caused your back pain which led to your dependence on prednisone. I recommend Metformin, working up to 2,000 mg per day, in divided doses. Metformin is first choice for diabetes, and is also a potent weight loss agent, as it restores insulin receptor sensitivity (See my article, “Metformin Update: Still the most effective Anti-Aging, Life Extension Drug” in Aging Matters Magazine, No. 4, 2013). Metformin is also a “multi-hormone receptor sensitizer,” so it will help your body to respond to all hormones (including cortisol, and its pharmaceutical “cousin,” prednisone), hopefully enabling you to reduce your prednisone dose somewhat.
I also recommend Acarbose. See my article “An Anti-Diabetic Weight Loss Agent” in Aging Matters Magazine, No. 2, 2015. The usual dose is 100 mg chewed with meals three times daily—but you can probably take a higher dose (perhaps up to 600 mg daily). I also recommend a third anti-diabetic drug, from the GLP-1 agonist class of drugs (Byetta, Victoza, ByeDureon, Trulicity, or Tanzeum). These medications are frightfully expensive, but may be covered by your insurance, or you may qualify for patient assistance from the manufacturer.
None of these three anti-diabetic drugs (Metformin, Acarbose, or the GLP-1 agonists) will cause hypoglycemia. They will normalize your glucose and insulin, and help you with weight loss.
In addition, I recommend an appetite-suppressant. I prefer the short-acting phendimetrazine, 35 mg three times/day, although you may need more due to your size. Also, since you are taking Lasix (furosemide) for water retention, I recommend enough to additional potassium and magnesium.
Also, how is your thyroid status? You may be hypothyroid, in which case an appropriate dose may normalize your metabolism. See “The Hypothyroid Epidemic” by Dr. Rick Wilkinson in Aging Matters Magazine, No. 4 2014.
I also recommend that you take a high potency Vitamin K complex. Chronic prednisone consumption can have a devastating effect on your bone density. Vitamin K2 (MK-4) is considered a drug for osteoporosis in Japan, in a dose of 45 mg/day.
Finally, back to your original question. Yes, Sermorelin may help, after you have instituted all of the above. It will help with maintenance of lean body mass, and will facilitate fat loss. But I believe we need to correct the underlying problems that got you where you are.
Many of these recommendations will require the cooperation of your physician. I hope he will consider them and agree. Please stay in contact and let me know how you are doing.
Ward Dean, MD
My aunty is suffering from chronic colitis since she had pelvis radiation, I would like to know what products from your company she can order to improve her health. I am looking forward to hearing from you soon. Thank you,
B.A.P., India
You didn’t say why she had the radiation, but if it was for cancer, then I recommend Low Dose Naltrexone (LDN), 4.5 mg per day, as an adjunct to any treatment she may be receiving. (1) LDN has also been shown to be of benefit for Crohn’s disease, (an inflammatory bowel disease). (2-3)
I also suggest Symprove®, it’s a superior, clinically-tested probiotic that will help to normalize many bowel-related symptoms. (4)
Ward Dean, M.D.
References
- Berkson BM, Rubin DM, Berkson AJ. Revisiting the ALA/N (alpha-lipoic acid/low-dose naltrexone) protocol for people with metastatic and nonmetastatic pancreatic cancer: a report of 3 new cases. Integr Cancer Ther. 2009 Dec;8(4):416-22.
- Weinstock LB. Naltrexone therapy for Crohn’s disease and ulcerative colitis. J Clin Gastroenterol. 2014 Sep;48(8):742.
- Segal D, Macdonald JK, Chande N. Low dose naltrexone for induction of remission in Crohn’s disease. Cochrane Database Syst Rev. 2014 Feb 21;2
- Fredua-Agyeman M, Gaisford S. Comparative survival of commercial probiotic formulations: tests in biorelevant gastric fluids and real-time measurements using microcalorimetry. Benef Microbes. 2015 Mar;6(1):141-51. doi: 10.3920/BM2014.0051.
I am a 40-year old woman, in otherwise good health and fit. But I have recurring skin problems, specifically acne and boils which not only appear on my face, but other parts of my body such as my back. Obviously this is not a pleasant experience for me, I have tried using fiber and vitamin C to help detox myself with some limited success, but I would welcome your advice.
N.M., England
Of course, I’m at a disadvantage in not being able to ‘eyeball’ your lesions. Skin lesions as you describe could be due to Rosacea, acne, or even by infectious microbes like staphylococcal bacteria. With that caveat, here are some general suggestions.
Vitamin D is essential for healthy skin, and a healthy immune system. Most of my patients are deficient in this essential vitamin. I like to see levels in the range of 60-70 ng/ml. To reach these levels usually requires supplementation of 5,000-10,000 IU per day. IAS has a very potent form of Vitamin D, D3-Pro, in a dose of 50,000 IU, these capsules should be taken once per week. [Ed- IAS now also stocks D3-5000 which are 5000 IU capsules).
Tetracycline or doxycycline may help. The usual dose of doxycycline is 100 mg twice per day. You may have to continue to take smaller ‘suppressive’ doses on a chronic basis, if you find that this will control your outbreaks.
Another suggestion is to purchase a bottle of ‘hand sanitizer’—basically an ethyl alcohol gel, and apply it topically to the skin several times daily. This will kill bacteria on the skin, and should help to ‘dry up’ your lesions.
If you have acne, you may apply Retin-A® topically, as well—although if you are truly having ‘boils’ (i.e., abscesses), Retin-A® will probably not be effective.
Finally, have you had your hormone levels tested? Excess testosterone (as can occur if you are taking DHEA—women very efficiently convert DHEA to testosterone) is known to cause acne in women. If you are taking DHEA, I’d suggest reducing your dose.
As I have gotten older I find that my sleep quality has appeared to have worsened. Now as a 70-year old woman I find that it’s not just the quality of the sleep but the time also. I am now at the point where I seem to be sleeping on average about 4 hours a night. What procedures can I follow to improve this and are there any sleeping drugs you recommend?
G.M., Australia
In Aging Matters™, Issue #1, 2013, I answered a similar question, and suggested the anti-seizure drug, Gabapentin (Neurontin®), as a powerful sleep aid. Gabapentin is an analog of the ‘notorious’ GHB. GHB is actually the safest, most non-toxic, non-habit forming sleep inducing agent there is. It is a natural substance, existing in every cell in our bodies in small amounts. When taken in adequate doses, it induces sound, restful sleep—enhancing all four phases of sleep—and is metabolized into harmless carbon dioxide and water.
My experience with gabapentin as a sleep inducing agent is excellent. Although gabapentin doesn’t work for everyone, most of my patients gratifyingly report that it causes sound, restful sleep, without frequent early-morning awakenings. When taken in an appropriate dose, at the proper time, there is little to no ‘hangover’ effect. If you experience a hangover, take it an hour or so earlier, or reduce the dosage. Dosages of gabapentin must be individualized. Some very sensitive people find as little as 300 mg to be adequate. Usually, however, 600-800 mgs are effective and some highly resistant patients require 900-1200 mg. It is a very safe, non-habit forming medication. IAS now stocks gabapentin.
My blood pressure seems to be rising, it used to be often 120/80, now it appears to be often around 140/90 – furthermore my resting heart rate can sometimes be around 90 beats per minute. I avoid caffeine and whilst I am overweight I am not obese and do mild exercise regularly. I am a 55 year old man.
F.M., Missouri
Although there are several nutrients that may lower blood pressure, the combination of high blood pressure with increased heart rate is best treated with a beta blocking anti-hypertensive medication. Propranolol (Inderal®) is good, although cardio-selective beta blockers like Atenolol®, Labetalol®, Carvedolol® or Metoprolol® are also excellent. These medications act to slow the heart rate, (I prefer a resting rate of 65-75 BPM), while simultaneously normalizing blood pressure. Start with low doses, and gradually increase the dose until the target heart rate is obtained. Naturally, please discuss these recommendations with your physician.
I recommend first normalizing your pressure (and heart rate) with one of these medications. You may also add a combination of potassium and magnesium for longer term use, which may enable you to wean yourself from the medication. I often prescribe magnesium-potassium aspartate as a source for these two minerals. The dose can be gradually titrated up to bowel tolerance (magnesium in high enough doses will cause GI distress and diarrhea)—but before that point is reached, blood pressure will usually return to normal.
In addition to monitoring your blood pressure, another useful parameter to follow is your Arterial Stiffness Index (ASI). ASI is one of the best biomarkers of biological aging, as documented in my book, Biological Aging Measurement—Clinical Applications. At the time the book was published (1988), only the most sophisticated cardiovascular testing labs had the expensive equipment required to conduct this test. In recent years, the folks at IAS discovered a compact, computerized unit that was affordable for Doctors’ offices (Bio-Clip™), and have now added a personal unit suitable for home use (Bio-Cuff™).
I am so pleased to be asking a world expert this question! Dr. Dean I would say that my memory and cognition as a 60-year old female is quite good and I take care to exercise my brain and use some of the nutrients that you recommended in your Smart Drug books. My main problem seems to be the speed of my recall; my recent conversations have too many ums and errs in them, much to my embarrassment, especially since I give a lot of presentations to my board. Please recommend something that might be able to help me.
M.R., Illinois
Not knowing what you are already taking makes this somewhat of a ‘guessing game,’ as I’m not sure what you are taking that isn’t working. Nevertheless, it sounds as if you’re looking for something that will offer a rapid effect that you will notice. If this is the case, I suggest alerting agents such as adrafinil or modafinil. Another cognitive-enhancing substance that has a rapid onset is vasopressin, available as either desmopressin (Minirin®) or Vaso-Pro™. These products are administered as nasal sprays, with rapid absorption through the nasal mucosa.
Vinpocetine, which acts to increase glucose uptake and oxygen utilization in the brain, also seems to cause rapid subjective improvements, sometimes perceived as brighter colors and improved hearing.
Centrophenoxine is another mild cerebral stimulant, although I usually think of it as being of long-term benefit for its ability to remove the cell-clogging lipofuscin, or aging pigment. Also, not to be overlooked, are the nootropics, of which Nootropil® (piracetam) is the prototype. This class of cognitive enhancers is known for improving communication between the cerebral hemispheres.
Have you considered the possibility of sub-clinical hypothyroidism? This may sometimes manifest in the symptoms that you describe. I suggest discussing this with a knowledgeable physician, who may recommend thyroid hormone for its cognition-normalizing effects.
I’m sure I may have recommended some substances that you may already be using, but hopefully you’ll find something within these recommendations that will restore your fluency.
I am a 48 year old male and over the last couple of years have noticed that my erections are becoming weaker, to the point where, although not diagnosed, I am sure that I have erectile dysfunction. I don’t really want to become reliant on taking a Viagra® pill every time my wife and I have sex, what can you recommend Dr. Dean and what may address the cause of this problem rather than just the symptoms?
S.S.K., Canada
First, I suggest that you ask your physician to check your testosterone levels. If they are in the low or low-normal range, you might ask him to prescribe testosterone. I prefer injectable testosterone (cypionate or enanthate) usually 200 mg injected intramuscularly every 2-3 weeks. Alternatively, the topical creams or gels may also help, although I believe topical testosterone is not as effective as the injectable route. That may solve your problem.
Another approach, in this regard, is IAS’s new Andro-Pro™. It is designed to naturally raise testosterone levels, although I have not had any clinical experience with it yet. However, there are several nutritional alternatives to Viagra® and the other phosphodiesterase (PDE-5)-inhibiting drugs like Cialis® and Levitra®, all of which are designed to increase the production of endothelium-derived nitric oxide (NO), one of the most important signaling molecules in our bodies. Nitric oxide was designated ‘Molecule of the Year’ by the journal, Science, in 1992, and a Nobel Prize in Physiology or Medicine was awarded in 1998 for its discovery. Unfortunately as we age, we lose our ability to produce NO. This puts us at risk for a host of conditions, including hypertension, atherosclerosis, myocardial infarction (i.e., heart attacks), stroke, Alzheimer’s disease, and erectile dysfunction.
One way to increase NO is to consume the nitric oxide-producing amino acid, arginine. The effect of oral arginine intake to improve erectile response was first investigated in animal models. Older rats supplemented with arginine resulted in increased nitric oxide synthase activity and increased nitric oxide levels, which caused improved erectile response. The authors of the study suggested that dietary supplementation with arginine might lead to improved sexual performance in humans, as well.
The first evidence that oral supplementation with arginine might lead to improvement in human sexual function came from a short-term study in 1994. The study showed a positive correlation between arginine supplementation and sexual performance and satisfaction.
These intriguing findings were supported by a more recent, larger study conducted at the Department of Urology and Nephrology at Tel Aviv University in Israel. Fifty men with confirmed erectile dysfunction were administered either a placebo or 5 g/day arginine for six weeks. Thirty-one percent of the subjects receiving arginine reported improvement and satisfaction in their sexual performance. In the placebo group, only 12% of the men noted improvement in sexual function. Importantly, at the 5 gram daily dose, no significant side effects occurred in any of the patients throughout the entire duration of the study. The percentage of patients reporting improved performance (31%) may not sound like an impressive number, but keep in mind that up to 50% of Viagra® users report no benefit from taking this prescription medication.
As a source of arginine, IAS offers Nitric-Pro™ powder, which contains a hefty 3500 mg of L-arginine plus magnesium (to help relax the smooth muscle layer of the endothelium), per serving.
Unfortunately, the intestinal enzyme, arginase reduces the effectiveness of the conversion of oral arginine to NO by metabolizing arginine, reducing the amount that is available for conversion to NO. Citrulline may offer a solution. Citrulline is a semi-essential amino acid that is not found in the diet- it is synthesized in the body via a mechanism called the urea cycle. In this metabolic pathway, arginine is catalyzed by the enzyme arginase to urea and ornithine. Ornithine, in turn, is converted to citrulline, which is converted to argininosuccinate, which is converted back to arginine, completing the cycle. It has recently been shown that oral citrulline supplementation increases the plasma arginine concentration and augments NO-dependent signaling in a dose-dependent manner. This provides the rationale for using oral citrulline supplementation as a donor for the arginine/NO pathway in those with ED.
An article in Urology described a pilot trial aimed to determine whether oral citrulline supplementation could improve erection hardness in patients with mild ED. In the Urology study, 24 men (mean age of 56.5 ± 9.8 years) with mild ED (erection hardness score [EHS] of 3) received a placebo for 1 month. They were then given citrulline, 1.5 g/day split into two doses, for another month. At the end of the study, the erection hardness score, number of intercourses per month, treatment satisfaction, and adverse events were recorded.
The improvement in the EHS from 3 (mild ED) to 4 (normal erectile function) occurred in 2 (8.3%) of the 24 men when taking placebo during the first half of the study. But when the subjects were switched to citrulline, 12 (50%) of the 24 men reported achieving an EHS of 4. An EHS of 3 is considered “hard enough for penetration but not completely hard,” while an EHS 4 is “completely hard and fully rigid.” citrulline increased hardness by 50%. At the same time, the mean number of intercourses per month increased from 1.37 at baseline to 1.53 at the end of the placebo phase (about 12% greater frequency) and 2.3 at the end of the treatment phase (about a 68% increase) for citrulline. Citrulline increased successful intercourse connects by 56% more than placebo, and all patients reporting an EHS improvement from 3 to 4 reported being very satisfied.
Perhaps the most effective way to increase nitric oxide has recently become available. It is a patent-pending combination of natural products, developed at the University of Texas Health Science Center, called Neo40®. Neo40® is primarily a combination of nitrate-rich beet root, and nitrate reductase activity-enhancing Hawthorn Berry extract, plus a relatively small amount of citrulline.
Preliminary clinical studies at the Houston Institute for Clinical Research indicate that Neo40® has demonstrated clinically relevant increases in NO and serum nitrate concentration, improvement in triglyceride levels, and normalization of blood pressure in hypertensive patients. Anecdotal reports from my patients who have used Neo40® also include rapid relief from angina attacks, and Viagra-like enhancement of sexual performance.
Another approach to improving erectile dysfunction is the time-honored multi-purpose herb, Ginkgo biloba extract (GBE). In a 1991 study, fifty patients with proven arterial erectile impotence were treated with 240 mg of GBE daily for nine months. The patients were divided into two groups. The first group had achieved sufficient erections with intracavernous papaverine injections before beginning treatment with GBE. The second group had not achieved sufficient erections with high-dose papaverine injections.
In the first group (n = 20), all patients regained spontaneous and sufficient erections after six months of oral GBE treatment. Arterial flow rates were actually improved after three months and continued to improve at six months. Rigidities at the penile tip and base were significantly improved after six months and remained constant during the nine month duration of the study. In the second group (n = 30) (this was the group that did not respond to high-dose papaverine injections—i.e., a very severe state of ED), improved arterial penile flow rates and rigidities were noted at six and nine months. Nineteen patients, responded to intracavernous PGE1 following GBE treatment. Of these 19 patients, 9 required a minimal dose of 5 mcg PGE1, while the other 11 required a maximal dose of 20 mcg. The remaining 11 patients remained impotent. Thus, it appears that Ginkgo biloba extract at a dose of 240 mg per day may also greatly assist those with ED.
In summary, I recommend evaluation of testosterone levels, and replacement, if appropriate, or using Andro-Pro™, arginine (3-5 grams per day) or the arginine-containing Nitric-Pro™, citrulline (1.5 grams per day), Neo40® (1 tab twice daily), and Ginkgo biloba (240 mg per day). I don’t recommend starting everything at one time—rather, begin with one nutrient at a time, and add other nutrients in sequence so you can tell what is (and is not) working.
1. Moody JA, Vernet D, Laidlaw S, Rajfer J, Gonzalez-Cadavid NF. Effects of long-term oral administration of L-arginine on the rat erectile response. J Urol 1997;158: 942-¬7.
2. Zorgniotti AW, Lizza EF. Effect of large doses of the nitric oxide precursor, L-arginine, on erectile dysfunction. Intl J Impot Res 1994;6:33-¬5.
3. Chen J, Wollman Y, Chernichovsky T, Iaina A, Sofer M, Matzkin H. Effect of oral administration of high-dose nitric oxide donor L-arginine in men with organic erectile dysfunction: results of a double blind, randomized, placebo-controlled study. BJU Int 1999;83: 269¬-73.
4. Cormio L, De Siati M, Lorusso F, Selvaggio O, Mirabella L, Sanguedolce F, Carrieri G. Oral citrulline supplementation improves erection hardness in men with mild erectile dysfunction. Urology 2011 Jan;77(1):119-22.
5. Janet Zand, Frank Lanza, Harsha K. Garg, and Nathan S. Bryan. All-natural nitrite and nitrate containing dietary supplement promotes nitric oxide production and reduces triglycerides in humans. Nutrition Research, 31 (2011) 262-269.
6. M. Sohn M and R. Sikora. Ginkgo biloba extract in the therapy of erectile dysfunction. J Sex Educ Ther (1991) 17: 53-61.
I have recently been given a urine challenge test and discovered that I am ‘high’ in cadmium and ‘moderately high’ in mercury. What might be the best types of chelation (oral and IV) that I can use to excrete these toxic heavy metals and how long may I have to do so?
R.K., Georgia
Intravenous EDTA is an excellent chelator of cadmium, and fairly good chelator of mercury. A minimum of ten treatments will be required, although more will undoubtedly be better. If intravenous EDTA is not available in your area, oral treatment will also help—and is also a useful adjunct if IV treatment is used. One alternative is Dr. Gordon’s Beyond Chelation Improved®. Another oral treatment, (perhaps the best chelator of mercury) is DMSA (dimercapto succinic acid). I recommend a conservative protocol of 300 mg of DMSA orally every other day.
Zeolite is another very interesting chelator worthy of consideration.
Unfortunately, heavy metals are usually lodged in the bones and the brain. Chelation therapy detoxification is a prolonged process, as the chelating agents normally bind with the heavy metals in the blood, lowering the blood levels of these substances, which then re-equilibrate from the bones and brain to restore the levels in the blood. Thus, repeated treatments are required to ultimately deplete the ‘stores’ in the bones and brain. Dr. Gordon believes this should be a lifelong process.
(Ed. – DMSA can be found in Detox-Pro™ at 100 mg per capsule. High quality Zeolite is available in liquid mouth spray and dissolvable in water capsule – see Advanced Cellular Zeolite® and ZeoGold® for details).
I appear to have reoccurring bouts of gout which has now become more painful and uncomfortable. I would very much like to know how I can rid myself of this problem.
E.M., Colorado
Of course, you should avoid foods that trigger your attacks, such as red meat, shellfish and alcohol. Colchicine is the time-honored treatment for acute flares of gout, but due to FDA interference, has now been made a frightfully expensive prescription drug in the U.S.
Fortunately, IAS has located an affordable version of colchicine in 1 mg tablets. Take 1 tablet at the first sign of a gout flare, then 1 more 2 hours later if still symptomatic. Wait 12 hours before taking a third dose, if it is needed.
Unfortunately, gout is a genetic illness, so there is no way to ‘rid yourself of the problem.’ However, with proper diet and judicious use of colchicine, the discomfort can be prevented or greatly alleviated.
My doctor has prescribed a statin (Lipitor®) to lower my cholesterol level. Friends have told me that I should also take CoQ10; I would like to know your opinion.
G.P.R., Texas
I believe that statin drugs such as Lipitor® are not a preferable solution to hyperlipidemia. Statins are literally toxic to the muscles, and result in weakness, fatigue, cramps, and in worst cases, destruction of the muscle (rhabdomyolysis). These side effects are well known to most cardiologists. As you suggested, statins also impede the actions / reduce body concentrations of CoQ10. Consequently, CoQ10 has been suggested to be taken whenever statins are given.
So yes, I agree with your friends who recommend CoQ10—IF you feel you must take statins.
However, as I said above, the safest, most non-toxic, cheapest lipid lowering substance known is NIACIN (vitamin B3). Niacin lowers total cholesterol, triglycerides and LDL and RAISES HDL.
Recently, there has been a negative report about niacin — however what is NEVER mentioned is that the negative report involved NIA-SPAN® — a prescription form of timed-release niacin. Timed-release niacin is known to be toxic. Therefore I recommend the cheaper health-food store variety of Nicotinic Acid, or the non-flushing Inositol Hexanicotinate or Xanthinol Nicotinate forms.
[Ed. – IAS provides niacin in Beyond Chelation Improved® and Xan-Pro™ which is the most potent form of niacin called xanthinol nicotinate].
My rising from bed temperature seems to be regularly below 36° C (96.8° F). I can recognize signs of hypothyroidism in myself. Can you please advise what dose of thyroid I should use to raise my morning temperature with either a T3 or natural thyroid supplement?
B.D., Switzerland
I usually recommend Armour® Natural Thyroid, rather than pure T3. Armour contains the naturally-occurring range of thyroid hormones—T2, T3, and T4—and seems to have more beneficial effects than the commonly used T3 (Synthroid®).
Temperature is important—but even more important is your heart rate. I like to maintain the resting heart rate in the 65-75 beats per minute range. I usually start my patients on no more than 1 grain (60 mg) of Armour® thyroid. If needed, I adjust the dose up or down depending on the response. Response to the dosage used is more important than the results of any thyroid function blood tests—which in most cases are a ‘waste of blood.’ If the pulse rate and temperature remain normal, and the patient feels well, there is very little likelihood of overdosing on thyroid. I try to treat the patient—not the blood test.
I am very interested in the mitochondrial theory of aging and understand that healthy mitochondria will generate good internal energy levels and repair systems. Could you please recommend any products that may help my mitochondria perform better?
J.J., New Jersey
There are two approaches to enhance mitochondrial energy production.
First, is to optimize the mitochondrial energy producing intermediates such as D-Ribose (5 grams per day), Creatine (5 grams per day), CoQ10SR™ (100 mg per day), NADH and IAS’s ATP-Boost™ (which is principally a combination of Acetyl-L-Carnitine, Alpha Lipoic Acid and Adenosine Triphosphate). The unique cognitive-enhancing drug, Hydergine, has also been shown to restore mitochondrial function of old animals to that of more youthful counterparts.
The other approach to enhanced mitochondrial function is to increase the number of mitochondria. Studies have shown that youthful organisms respond to exercise by increasing the number of small, efficient, energy-producing mitochondria. With increasing age, mitochondria have fewer tendencies to increase in number; rather they increase in size, but are less efficient energy-producers. Recently, a new substance, (PQQ) has been shown to regenerate small, efficient mitochondria — essentially as in youthful organisms.
Thus, the ideal mitochondrial restoration formula would seem to be a balanced combination of mitochondrial energy producing intermediates, PLUS the new mitochondrial regenerating supplement, PQQ-Pro™.
(Ed. – Please note that 2 grams of D-Ribose are contained in each rounded teaspoon of Bio-En’R-Gy C®).
I have been diagnosed with angina. What can I do to alleviate this situation?
C.K., England
First, for acute (immediate) relief, I recommend a combination of IAS’s Nitric Pro™ and Neo40®. This combination will maximize the release of Nitric Oxide, essential for vasodilation and enhancement of blood flow to the heart and other organs. Also, I recommend one aspirin per day.
For long-term improvement, I recommend 1,500 mg of Niacin (vitamin B3) to normalize your lipid levels. Niacin is the safest, cheapest, most effective lipid-lowering agent there is. Also, 500mg of Turmeric (Ed. – or approximately 125mg curcumin) to normalize your fibrinogen levels, which is perhaps one of the most important markers of cardiovascular risk. I also suggest adding Dr. Garry Gordon’s Beyond Chelation Improved®, which contains EDTA. In addition you can consider 100 mg of CoQ10SR™ and IAS’s unique formula for cardiac support, Cardio-Pro™. Let me know how you do.
I would like to know if there are supplements particularly good at helping mild forms of depression. I don’t have anything to be depressed about, but some days I don’t feel like getting out of bed.
D.R., Florida
Taking your question at face value, without considering the myriad of potential causes, I’m guessing that your sleep is not as restful as it possibly could be. Tryptophan (1500-2,000 mg) or 5HTP (150-200 mg) at bedtime have sleep-inducing and antidepressant effects. IAS carries both of these nutrients. Also, melatonin (3-6 mg) can be taken along with tryptophan (or 5HTP). Neurontin® / gabapentin, as mentioned above, is an excellent sleep-inducer when used in appropriate doses—and GHB (of which Neurontin® is a chemically-related analog) is a superior antidepressant. When taken in appropriate doses, Neurontin® results in very restful sleep, and enables one to awaken refreshed, and literally ‘bounce out of bed’ (similar to the sleep-wake profile of GHB). Hypothyroidism can also be a cause of low energy and depression so please see my response to the question above.
Dr Dean,
I have your book the GHB, the Natural Mood Enhancer, which is a great resource for anyone who wants to learn about this remarkable substance – but which has sadly been banned in many parts of the world. When it was legal, I was able to use it very successfully for helping me sleep. I am not ‘officially’ an insomniac, but consider myself borderline. Is there anything similar to GHB that I could try, (legally of course) that you can suggest that will help me get better sleep at night?
A.B., Australia
Neurontin (gabapentin) is a GHB analog, which is approved by the FDA as an anti-seizure medication, and also for fibromyalgia, restless legs, and nerve pain due to diabetic neuropathy and shingles. The most common ‘side effect’ of Neurontin® is ‘somnolence’ (i.e., it will induce sleep, in appropriate doses). It is a very safe drug, used in doses as high as 3.4 grams/day. Usually, restful sleep will result from doses ranging from 600-1800 mg about an hour before bedtime.
Another related substance is GABOB (gamma amino hydroxy butyric acid), available in 500 mg tablets as Gamibetal®. Gamma amino hydroxy butyric acid is also in Gamalate (at 37 mg) along with GABA (75 mg), magnesium and B6. IAS also stocks 5HTP (50 mg capsules), L-tryptophan (500 mg capsules) and melatonin tablets (3 mg), which also may help restore your sleep to normal.
I’m currently using 2400 mg of Nootropil® / piracetam daily to help me in my studies. Some days I get very focused clarity, but other days I don’t seem to achieve as much as I’d like to. I was wondering why this might be – do I need to adjust my dose or might I be better off on another piracetam related supplement? I would appreciate any advice.
S.P., New York
Frankly, I haven’t noted much difference between the various Nootropics (piracetam, aniracetam, pramiracetam, etc.) when taken in equipotent dosages. Therefore, I don’t think further increase in your dosage of Nootropil® / piracetam, or switching to one of the other piracetam analogs would result in further improvement. Instead, I would add one or more cognitive enhancers that act via different mechanisms, such as vinpocetine, which increases cerebral oxygen uptake and glucose metabolism, centrophenoxine (Lucidril), or the relatively fast-acting desmopressin nasal spray [Ed.- as mentioned above]. Another ‘wake up’ antidepressant cognitive enhancer is deprenyl / selegiline – especially, the fast-acting sublingual drops.
[Ed.- IAS provides piracetam / Nootropil® 800 mg tablets, plus in liquid form, aniracetam / Ampamet® in 750 mg tablets and a generic Ani-Pro™ in 750 mg capsules, pramiracetam in 300 mg capsules, vinpocetine/ Intelectol® in 5 mg tablets, centrophenoxine in 250 mg tablets and deprenyl (Dep-Pro™) in 20 ml/ 300 mg liquid with 1 drop = 1 mg].
Dear Sir,
I have high triglycerides, high homocysteine, and a low metabolism. I find myself rather lethargic and gaining weight. Could you please suggest any products that you feel may benefit me in my situation?
A.P.M., Great Britain
The safest, cheapest and most effective substance to normalize one’s lipid profile is nicotinic acid (niacin, vitamin B3). Niacin has the optimal effect on the lipid profile. It lowers total cholesterol, triglycerides, and LDL, and raises HDL (the so-called ‘good’ cholesterol). Most people will only require 1500-2000 mg of niacin per day, although I’ve used doses up to 6 grams per day.
[Ed.- IAS provides niacin in Beyond Chelation Improved® and Xan-Pro™ which is the most potent form of niacin called xanthinol nicotinate].
Another substance that normalizes triglycerides is the anti-diabetic drug, metformin. I’ve written on the antiaging benefits of metformin (a ‘metabolic rejuvenator’), as well as its weight-normalizing effects. As a key component of my often-prescribed weight loss protocol, my patients invariably report that after taking metformin, they feel better, have more energy, and lose their carbohydrate cravings. Also, they often are surprised to find that their clothes fit better, even before they note any loss in body weight. This is because metformin seems to cause a shift in body morphology—i.e., loss of body fat, and increase in lean body mass (bone and muscle). Bone and muscle are heavier than fat, resulting in a seemingly paradoxical increase in weight, despite significant fat loss.
[Ed.- IAS provides metformin in 500 mg tablets or Dianben® in 850 mg tablets].
Another frequent cause of the symptoms that you describe – fatigue and weight gain – is overt or sub-clinical hypothyroidism. Thyroid hormone is a natural substance that belongs in your body. I pay very little attention to thyroid blood tests. In most cases, I believe they are a ‘waste of blood.’ I prefer to treat my patients’ symptoms. If my patients exhibit a spectrum of hypothyroid symptoms, (i.e., cold hands and feet, low body temperature, depression, constipation, fatigue, or difficult weight loss), I start them on a low dose of thyroid (i.e., ½ to 1 grain of Armour® Thyroid), and gradually increase the dose every month or so, based on one’s clinical response. As long as the heart rate remains in the normal range (60-75 beats per minute), and the patient feels well, I believe there is very little chance of excessive thyroid being consumed.
The single best treatment for elevated homocysteine is anhydrous betaine (trimethylglycine – TMG), in a daily dose of 3,000-5,000 mg. Another advantage of TMG (besides lowering homocysteine) is that it converts to the antidepressant, SAMe. While SAMe is fairly expensive, TMG is amazingly cheap. Besides, TMG tastes good, and can be added to virtually any beverage (milk, juice, coffee, etc).
[Ed.- IAS provides betaine / TMG in the Bio En-R ‘Gy C® powder drink].
Dear Dr Dean,
I enjoyed reading your interview in Issue 4, 2012 of the Aging Matters™ magazine regarding the use of smart drugs and nutrients. Indeed, I have your books at home! I have some confusion over one of the smart drugs that I personally like to use, and that is Vasopressin. It seems to now be available as both the synthetic version called desmopressin and the original porcine version of vasopressin. I was wondering if you could please tell me the difference between the two nasal sprays and if they may have any different uses / actions and which one you prefer?
S.B.J., California
Desmopressin (1-desamino-8-d-arginine vasopressin) is the synthetic version of the posterior pituitary hormone, vasopressin. Desmopressin is considered to be longer acting, and perhaps more potent than its natural analog, but the clinical results with each are variable. I don’t think there’s much difference in the two – i.e., those who respond favorably to one will probably have a similar response to the other. IAS has both versions available. Desmopressin nasal provides 5 mcg per spray, the usual dose is 20 mcg per day, whereas the vasopressin provides 10 IU per spray, the usual dose is 20-25 IU per day. The effective dose is highly individualized, and may be slightly more or less than those cited.
[Ed.- IAS provides desmopressin / Minurin® in 2.5ml = 25 sprays and vasopressin / Vaso-Pro™ in 5 ml = 50 sprays].
I am very interested in using the Can-C™ eye-drops to help fight my cataract – but how soon might I see positive results and what may I do in addition to speed things along?
R.M.F., Scotland
In my experience, 3-6 months is the minimum time to see improvement with Can-C™, although I have known people who have persisted, and did not see improvement until over one year had elapsed. Of course, the time required depends on the person’s diligence with the drops, and the degree of progression of the cataract at the time the treatment, (2-drops twice a day) was begun. The formulators of Can-C™ eye-drops also designed Can-C Plus capsules, as an oral adjunct to the eye-drops. Note: Dr. Babizhayev, the principal Can-C™ researcher, doesn’t recommend lutein (found in many ‘eye’ formulas), as lutein competes with same receptors as N-acetyl carnosine, and could down-regulate efficacy of the drops.
An alternative to Can-C™ capsules, would be to take L-carnosine itself, one of the principal (and I believe, most active) ingredients in Can-C™ Plus capsules.
Additionally, you might consider the AGE-breaking aminoguanidine. Several Japanese research teams have demonstrated the ability of aminoguanidine to inhibit or completely prevent the development of cataracts in two diabetes-prone rat strains. The first team used the Shumiya cataract rat (SCR). SCR is a hereditary cataract model in which lens opacity appears spontaneously in the nuclear and perinuclear portions at 11-12 weeks of age. The researchers found that oral administration of aminoguanidine (AG) strongly inhibited the development of lens opacification in SCR rats.
In another very recent study, the researchers used another strain, Spontaneously Diabetic Torii (SDT) rats. SDT rats have marked hyperglycemia and severe ocular complications. They evaluated the effect of the anti-AGE agent, aminoguanidine, on the development of diabetic retinopathy (DR) and cataract. Five SDT rats were treated with aminoguanidine (0.5 g/L in drinking water). During the duration of the study, ALL of the control rats developed cataracts, whereas NONE of the aminoguanidine-treated rats developed cataracts. These results were dramatically illustrated in the accompanying photographs (Figure 1). The researchers concluded that aminoguanidine had a strong inhibitory effect on diabetic ocular complications in SDT rats.
Although I have unfortunately not found any human studies to corroborate these findings in rats, aminoguanidine has been shown to be safe and effective in humans for a number of conditions, and I would expect it to have the same cataract-inhibiting effect in humans as it has in rats.
1. Mitsushi Inomata, Masami Hayashi, Seigo Shumiya, Seiichi Kawashima and Yoshimasa Ito. Aminoguanidine-Treatment Results in the Inhibition of Lens Opacification and Calpain-Mediated Proteolysis in Shumiya Cataract Rats (SCR). The Journal of Biochemistry, 2000 Volume 128, Issue 5, Pp. 771-776.
2. Fumihiko Toyoda, Akihiro Kakehashi, Ayumi Ota, Nozomi Kinoshita, Chiho Kambara, Hiroko Yamagami, Hiroyuki Tamemoto, Hiroto Ueba, Prevention of Proliferative Diabetic Retinopathy and Cataract in SDT Rats with Aminoguanidine, an Anti-Advanced Glycation End Product Agent. The Open Diabetes Journal, 2011, 4, 108-113
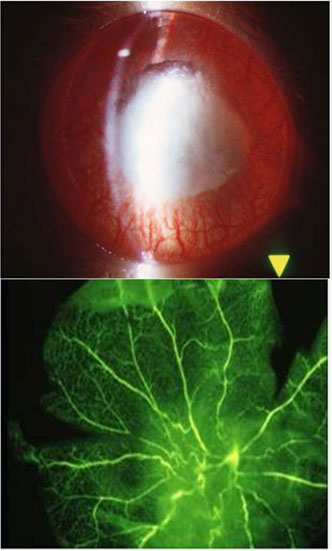
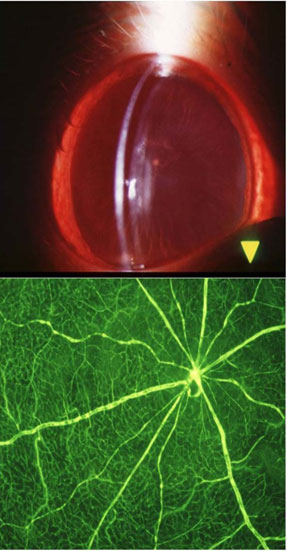
Figure 1, the Effect of aminoguanidine on diabetic cataract and retinopathy. The top row shows the slit-lamp findings in the lens. The untreated control rat has mature diabetic cataracts, whereas the aminoguanidine-treated SDT rat has minimal lens opacity. The bottom row shows the fluorescein angiomicroscopy findings. The untreated control rat has extensive fluorescein leakage and narrowing of the capillaries around the optic disc. The aminoguanidine-treated SDT rat has no abnormalities.
Dear Dr. Dean,
I have had issues with foggy thinking since my mid-40s. The rebalancing of my hormones has fixed about 50% of the fogginess. Also, I tried modafinil, and was amazed that I was able to think like I was in my 20s (I’m in my early 50s). Unfortunately, I developed hives pretty badly, and assume it was from the modafinil. So I ordered adrafinil from the IAS site. Do you know if it has the same sulfonamide profile as modafinil? I have sensitivity to sulfonamides, which is likely what brought on the rash.
P.H., Canada
Dear P.H.,
Unfortunately, you appear to have experienced an uncommon but potentially severe side effect of modafinil in those who are allergic to it- a profound rash (see figure two).

Figure two: A rare, but potential side effect of the Eugeroic drugs is a skin rash.
As you can see, the structures of adrafinil and modafinil are quite similar (see figure three). Consequently, you should avoid both of these medications.
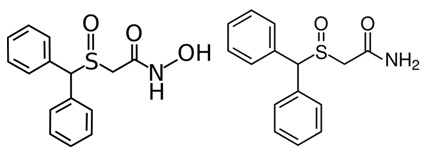
Figure three: The structure of adrafinil is shown on the left, the structure of modafinil is shown on the right; the close similarity between the two can be clearly seen.
Suggestions to replace these drugs include combinations of desmopressin or vasopressin nasal spray, piracetam (Nootropil®), phosphatidylserine, acetyl-L-carnitine, and Vinpocetine which should all be beneficial, but will unfortunately not give you the ‘instant’ alerting effects of modafinil or adrafinil.
Ward Dean, M.D
[Ed- Acetyl-L-carnitine is available in ATP-Boost™ from IAS].
Dear Dr. Dean,
I have been suffering from adrenal fatigue for several years, and took a round of the peptide bioregulator for the adrenal gland. I am perimenopausal and on bio-identical hormones. About 2-3 weeks after taking the bioregulators, I started having a period and my breasts were extremely tender. Is it possible that the adrenal surge also increased estrogen production in that short amount of time? I will have my blood tested in September for my hormone levels, but in the meantime my naturopath (hormone specialist) lowered my estrogen prescription by half, just based on my external symptoms.
What do you think?
M.B., United States
Dear M.B.,
Firstly, the Russian peptides are a learning curve for us all at present, although they’re based on very good science. They are a direct extension of the work of my Russian mentor, Prof. Vladimir Dilman, and many of his students.1 Dilman believed that a principle cause of aging was the progressive loss of central and peripheral hormone (and neurotransmitter) receptor sensitivity to negative feedback inhibition. Consequently, he proposed his revolutionary and underappreciated approach to antiaging therapeutics—i.e., to identify drugs and neuropeptides that are capable of restoring this altered receptor sensitivity to a more youthful state. He believed that metformin and phenformin, (a pharmaceutical predecessor to metformin) were the prototypes of these ‘metabolic rejuvenators.’
We’ve already received numerous positive testimonials of the actions of these biopeptides over very short periods of time, and in cases like yours, in very low doses. It appears that the Russian research is being borne out in patient reality. We recommend, (as you have done) that anyone on any type of hormonal therapy monitor themselves closely–especially while taking the peptide bio-regulators. Adaptation to one hormone can naturally affect others, too. Dilman demonstrated long ago that phenformin not only restored insulin receptor sensitivity, but that of cortisol, as well (see figure one).2
I believe that metformin also restores sex steroid receptor sensitivity, although this is merely my clinical impression.
It is not yet possible to say definitively whether adrenal changes due to the adrenal bio-regulators made this impact on your estrogen levels, (or the sensitivity of your estrogen receptors), but it is certainly likely that they did. It would be of value to know your before and after levels of your adrenal hormones (including DHEA), and their changes over 24 hours, as well as estrogen and progesterone. It is clearly a favorable sign that you are improving clinically while simultaneously lowering your estrogen prescription.
Ward Dean, M.D.
- Dilman, V., and Dean, W. The Neuroendocrine Theory of Aging and Degenerative Disease, Center for Bio-Gerontology, 1992.
- Ostroumova, M.N. Age-associated decrease in hypothalamic-pituitary complex sensitivity to dexamethasone suppression test. The effect of stress, epithalamin and phenformin. Probl Endokrinol, 1978, 24: 59-64.
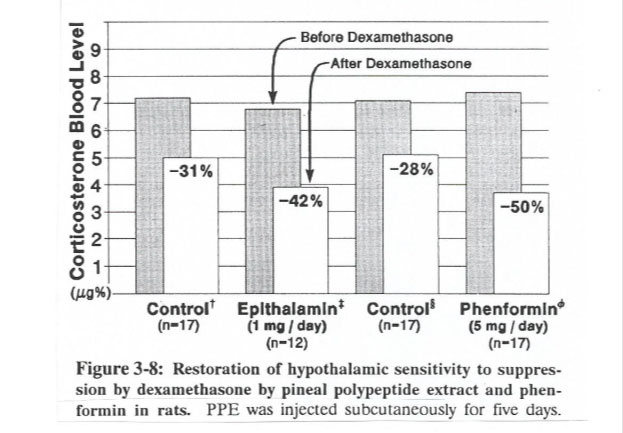
Figure One: Restoration of hypothalamic sensitivity to suppression by dexamethasone by pineal polypeptide extract, (epithalamion) and phenformin in rats. PPE was injected subcutaneously for 5 days, and Phenformin was injected intraperitoneally for 5 days. The results show that both PPE and phenformin restore hypothalamo-pituitary complex sensitivity to inhibition by dexamethasone (i.e., synthetic cortisol) (Dilman and Dean, 1992).
Hi, Dr. Dean, First I want to say, you are amazing. I love reading everything you have written on this site. I have Hashimoto’s. I live in Argentina, and Armour® thyroid is not available. I want to switch to Armour, as I have heard so many good things about it, and traditional medications are not helping me. My current combination is 100 mcg of Levetiroxina (T4) and 40 mcg of T3. How would you recommend I start with Armour? Thank you so much.
D.B., Argentina
Dear D.B.,
One grain (60 mg) of Armour® thyroid is roughly equivalent to 100 mcg of Synthroid® (Levetiroxina). Armour is comprised of a natural balance of T4, T3, and T2. Therefore, one grain would be a good ‘starting dose.’ Generally I suggest advancing the dose of thyroid by about ½ grain each month, until desired results are achieved. Although blood tests provide additional information, I adjust the dose primarily based on how the patient feels, body temperature, and most important, the heart rate. Shoot for a heart rate of 65-75, and try to maintain the resting heart rate in that range. If the heart rate begins to increase into the 80s, and especially the 90s, reduce the dosage to that where you feel well, but have a normal heart rate.
In your case, with Hashimoto’s, I’d also add anti-inflammatory herbs like turmeric, boswellia and berberine. Also, consider 2-8 drops per day of Lugol’s solution, (potassium Iodide).
Ward Dean, M.D.
[Ed- Curcumin is the extract of turmeric available in slow release form as CurcuminSR™ from IAS].
In the last few years my skin has developed ‘liver spots.’ Additionally, I have a diagnosis of Hepatitis C or B. Apparently there are often false positives in the testing. While my liver enzymes are slightly elevated they are not in the range of someone with the hepatitis C virus. The enzyme levels decrease with major autohemotherapy (using ozone). I have had several glutathione IVs, and I regularly do a gall bladder flush. What other therapies are available for liver health?
Thanks a lot, J.M., United States
Dear J.M.,
Firstly, ‘liver spots’ don’t have anything to do with liver disease. They are also known as ‘age spots,’ and are due to the deposition of ‘aging pigment’ (lipofuscin). Lipofuscin is a fluorescent, highly cross-linked lipoprotein pigment resulting from the inefficient metabolism of polyunsaturated fatty acids. Lipofuscin accumulates in our cells with age, and ‘liver spots’ in the skin are thought to be an indicator of the concentration of lipofuscin elsewhere in the body. Dr. Kalidas Nandy, of the Department of Anatomy and Neurology, Boston University School of Medicine, stated that; “One of the most consistent cytological changes in aging mammals, is the deposition of lipofuscin” (age pigment).1 Researchers in Italy emphasize that; “lipofuscin pigments are well known biomarkers of the aging process.”2
I believe that ‘liver spots’ are an indicator of the degree of lipofuscin accumulation in other parts of the body (brain, heart, muscles). Although there is no evidence that lipofuscin is in any way harmful, it can be considered as ‘intracellular garbage,’ and may in some way impair cellular function. Fortunately, there are a number of substances that can eliminate these pigments—and you can watch your skin changes as an indicator of the degree of their removal. Centrophenoxine, DMAE, and Hydergine, have all been demonstrated to reduce lipofuscin deposits in experimental animals1. I know several patients who have used these substances to rid themselves of their ‘age spots,’ over 3-6 months
I’m puzzled that you have a diagnosis of “hepatitis A or B.” With tests available today, very specific, accurate diagnoses can be made. If you really do have hepatitis, the type of hepatitis can accurately be made—and if you have hepatitis C, a ‘viral load’ (using PCR) will provide an indication of the severity of the disease. Liver enzyme tests are an indicator of liver abnormalities, but may be caused by other factors such as statins, acetaminophen (Tylenol®) or other drugs. I’d ask your physician to re-check, or find another doctor.
Nevertheless, to answer your specific question regarding substances that you can add to your ‘liver support’ program, I suggest vitamin B-12, N-Acetyl Cysteine (NAC), glutathione, carnitine, taurine and methionine, and the herbs milk thistle and turmeric.
Metformin, which is now recognized as the treatment of choice for Type 2 diabetes, and which I have long-recommended as a premier antiaging substance, has also recently been reported to be of benefit for those with hepatitis C and diabetes. In a study of 100 diabetics with hepatitis C, 26 of whom were treated with metformin, it was found that metformin use resulted in an 81% reduction in the risk of hepatocellular carcinoma and a 78% reduction in liver-related death or need for liver transplantation.3
Ward Dean, M.D.
[Ed- Curcumin is the extract of turmeric available in slow release form as CurcuminSR™ from IAS].
- Nandy, K., Mostofsky, D.I., Idrobo, F., Blatt, L. and Nandy, S. Experimental manip[ulations of lipofuscin formation in aging mammals. In: Lipofuscin—1987: State of the Art. I. Zs. Nagy, Editor, pp. 289-304, Elsevier Science Publishers, Amsterdam, 1988.
- Del Roso, A., De Tata, V., and Bergamini, E. Regional distribution of the age pigment accumulation across the free wall of the left ventricle of rat heart. In: Lipofuscin—1987: State of the Art. I. Zs. Nagy, Editor, pp. 441-442, Elsevier Science Publishers, Amsterdam, 1988.
- Nkontchou, G., Casson, E., Aout, M., et al. Impact of metformin on the prognosis of cirrhosis induced by viral hepatitis C in diabetic patients. J Clin Endocr Metab, 96: 2601-2608, 2011.
Two days ago I was diagnosed with Essential Tremor (ET). I am 37 years old and in good shape but struggle with tremors in my hands and at times in my feet. I also have anxiety from time to time.
I am looking for a line-up of supplements that I could try synergistically to possibly help restore cognitive health or at the very least stop any progression. Currently I am taking magnesium, idebenone, CoQ10 and creatine. I also am taking a prescription (today is my first day) of primidone…only half a pill to help control tremors. I avoid caffeine, as anything that “excites” the brain seems to make the symptoms worse. Please let me know what recommendations you have for me. I am willing to experiment with different things in an effort to find something that works.
Thanks, B.B., USA
Dear B.B.,
Why this condition is called essential is a mystery to me. The same with “essential hypertension.” There is nothing “essential” about either of these conditions. I guess it’s our way of admitting we don’t know the cause. Unfortunately, just as we don’t know the cause, there is also no universally effective treatment–although many substances have been tried. Some people respond better to one treatment than another. Consequently, a trial-and-error approach is used, to try to find something that will work with minimum side effects. Currently, Primidone (Mysoline®, Elan Pharma)—that you are taking–is a first-line choice. Primidone is an anti-epileptic structural analog of phenobarbital. In early studies of primidone in ET patients, beneficial responses were noted in 60%.
Another drug to consider is Propranolol (Inderal®, Wyeth Pharmaceuticals). Propranolol is a beta-blocker, and was the first medication shown to be efficacious for ET. Propranolol may be administered on either an as-needed (PRN) or a constant-use basis. Propranolol is beneficial in approximately 50% to 70% of patients with ET.
Primidone and propranolol may also be used in combination if either one alone has not sufficiently controlled the tremor. In addition, when appropriate, low dose benzodiazepines, such as lorazepam or clonazepam can be added to primidone and/or propranolol. As is the case with propranolol, benzodiazepines may be used in small doses on a PRN basis about 30 minutes to 1 hour before an important event.
Topiramate (Topamax®, Ortho-McNeil), used for migraine headaches, may also be tried for ET. Topiramate treatment improves tremor scores by approximately 29%, at an average dose of 300 mg.
The anticonvulsant gabapentin (Neurontin, Pfizer) has also been used in ET. Gabapentin monotherapy is comparable to propranolol in reducing tremors, and may have fewer side effects than many of the other anti-ET substances.
Calcium Channel Blockers like nicardipine (Cardene®, Roche) and nimodipine (Nimotop®, Bayer) have shown some promise in attenuating ET. However, these agents generally are less effective than propranolol.
For most ET patients, alcohol consumption may temporarily attenuate tremors. Therefore, a small amount of alcohol ingested before an important event may provide transient symptomatic relief.
Other substances that have been used with limited success in ET include low-dose amantadine (Symmetrel®, Endo Pharmaceuticals), clonidine (Catapres®, Boehringer Ingelheim), trazodone (Desyrel®, Bristol-Myers Squibb), thymoxamine, and linoleic acid.
Finally, you might investigate pulsed electromagnetic frequency (PEMF) for essential tremor. I’ve seen a number of unconfirmed reports of PEMF’s benefits for ET.
I know you asked for supplements that might help, and I gave you mostly a list of drugs. Hopefully, you may find something in this assortment that will control your tremors, without causing bothersome side-effects. In keeping with your objective to control your symptoms and restore cognitive health, my top two suggestions are to try Gabapentin, starting with 600 mg as a night-time dose, and PEMF.
Ward Dean, M.D.
I am most interested in the glycation theory of aging- whereby because of proteins cross-linking they become impaired etc. I am a 50 year old male who has been tested by BioCLIP™ and found to have hardening of the arteries. I also have mild cataracts and a potential pre-diabetic (type-II) development, (hence my interest in this theory!) Please advise me on any suitable strategies to reduce my glycated blood load.
B.A., Oregon
Dear B.A.,
The glycation theory of aging is a modern outgrowth of the venerable cross-linking theory of aging, first proposed by Johan Bjorksten in 1942.1,2 Bjorksten was a chemist from Finland, who earned his Ph.D. degree at the University of Wisconsin in 1937. He went to work for the Ditto Corporation of America, which was the ‘Xerox’ of the day.
Protein cross-linking as cause of aging
While at Ditto Corporation, one of the main problems Bjorksten faced was to develop a way to increase the ability of the Hectograph films to withstand summer temperatures, exposure to water, mechanical stretching and friction, and to prevent their drying out and cracking. The ‘aging’ of hectograph films was due to the cross-linking of protein molecules, which Bjorksten believed was also the cause of aging in humans. This was confirmed in a crude way by comparing the similarity between the shape of the mortality curve for humans (Fig. 1)
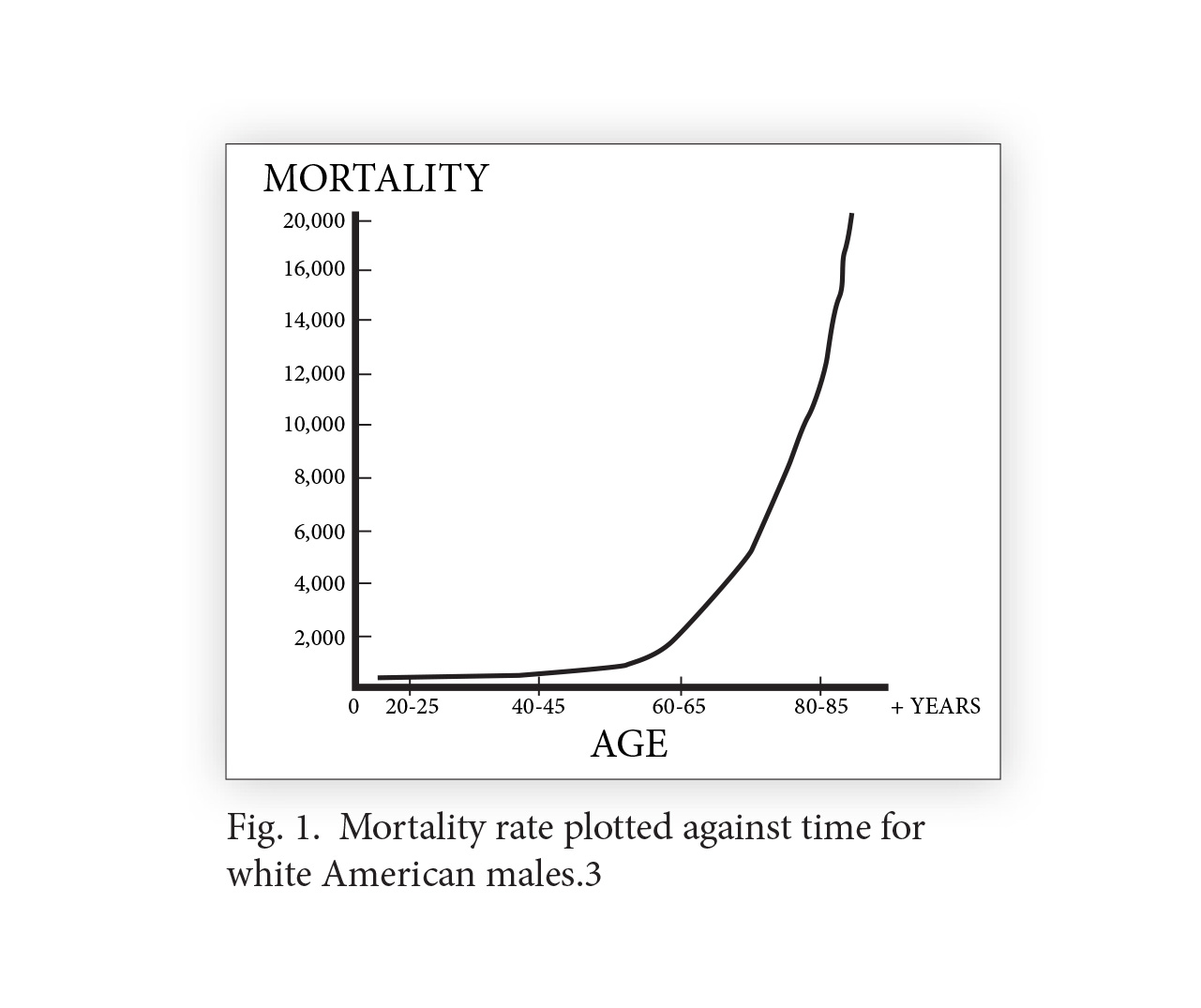
with a viscosity curve of gelatin during a cross-linking reaction (Fig. 2).3,4 The crosslinkage theory stated that the principal cause of aging was the linking together of two or more large molecules (macromolecules), which progressively linked with other molecules, impairing the functioning of cells, tissues, and organs, resulting in the aging of the organism.
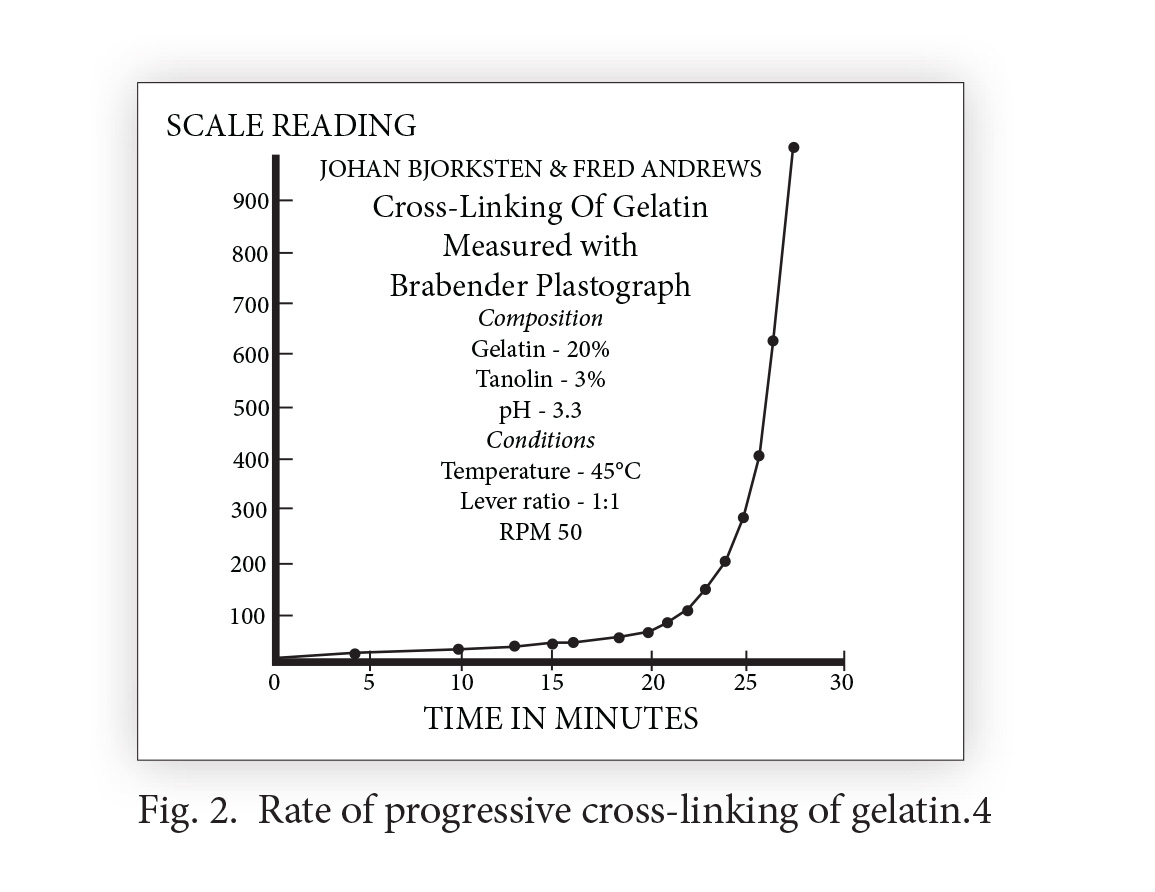
Search for cross-linkage inhibitors
Bjorksten focused on a potential means of preventing and breaking up crosslinkages by using chelating agents that attach to metals within the body, enabling them to be excreted. Ethylene-diamine-tetra-acetic acid (EDTA) is a synthetic amino acid that removes metal-based crosslinkages by chelation, thereby “depolymerizing the gerogenic aggregates.” 5 Chelating agents in current clinical practice besides EDTA (approved for use in the treatment of lead poisoning) are deferoxamine (Desferal® for acute iron intoxication), and DMSA (used to treat lead and mercury intoxication). Physician members of the American College for Advancement in Medicine (ACAM) are proponents of intravenous chelation therapy with EDTA as a treatment for many chronic degenerative diseases, like atherosclerosis, hypertension, diabetes, and Alzheimer’s disease.6 Chelation with oral EDTA chelation is also becoming more widely used.
[Ed. – EDTA is available in BCI®, Beyond Clean 2® and Beyond Fiber®]
Other natural chelators include garlic, 7 chlorella, 8 lactic acid, citric acid, and malic acid. Bjorksten demonstrated that lithium was also an effective aluminum chelator and crosslinkage inhibitor, stating that “lithium continues to be the most effective electrolyte for aluminum detachment.” 9
[Ed. – Lithium orotate is available from IAS]
Chelators as life-extending substances
A number of studies confirm that chelating agents, particularly, EDTA — may have life-extending properties. Scientists demonstrated the life-extending effects of EDTA on lowly rotifers (small multi-celled animals found in freshwater lakes and ponds).10-14 In the Soviet Union in the 1970s, Dr. T.L. Dubina performed a series of studies with EDTA on the life span of rats. In most of the studies, the mean life span of female rats treated with EDTA was increased by nearly 50%, and in one study the maximum lifespan increased 18-25% over the control animals. 15
Aluminum—a powerful cross-linker
Aluminum is a highly reactive metal that occurs freely in nature, and comprises over 8% of the earth’s crust. Although it also occurs very widely in human nutrition, (most people ingest 10-100 mg of aluminum daily), it does not play a role in any known metabolic process. Aluminum is highly toxic, even in extremely small amounts, and although the neurotoxic effects of aluminum have been known for many years,16 scientists have recently shown that aluminum accumulation may contribute to Parkinson’s disease 17 Down’s syndrome 18 and Alzheimer’s disease.19
Aluminum uptake increases with age
In 1955, during a talk on gelatin crosslinkages and aging at the Gerontological Society in Baltimore, Bjorksten discussed the relationship of aluminum to crosslinking. One of the attendees, Prof. H.H. Zinsser of Columbia University, was so interested in the concept that he and Bjorksten began a fruitful collaboration that was to last for seven years. Using spectrographic analysis, they examined the aluminum content of 84 persons, ranging in age from 10 to 90 years (Fig. 3).
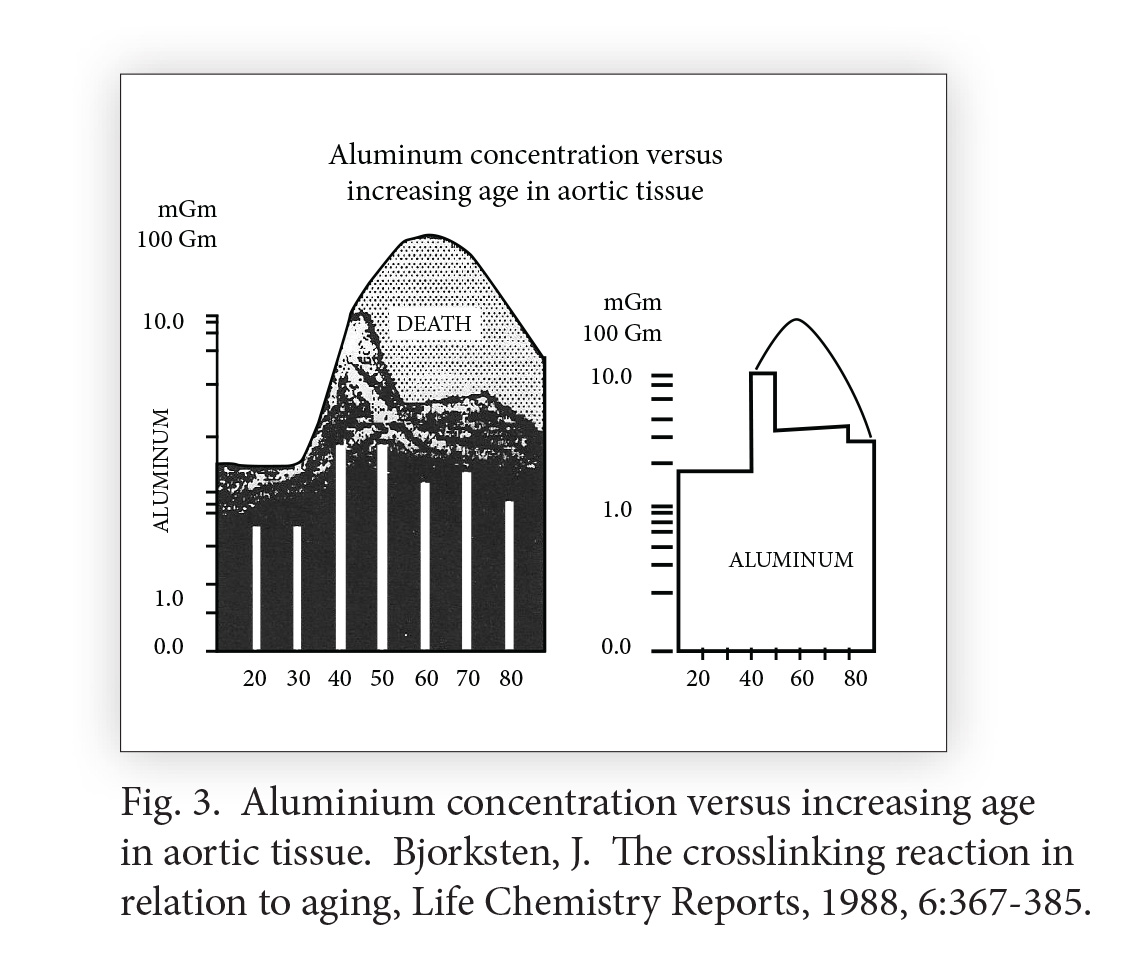
They found peak levels at age 40-50, followed by a drop and then leveling off, indicating that those whose aluminum accumulation peaked in middle age most likely did not survive the next ten years. 20 Zinsser’s data were confirmed independently by scientists who demonstrated a progressive increase of aluminum concentrations in the brain (Fig. 4).
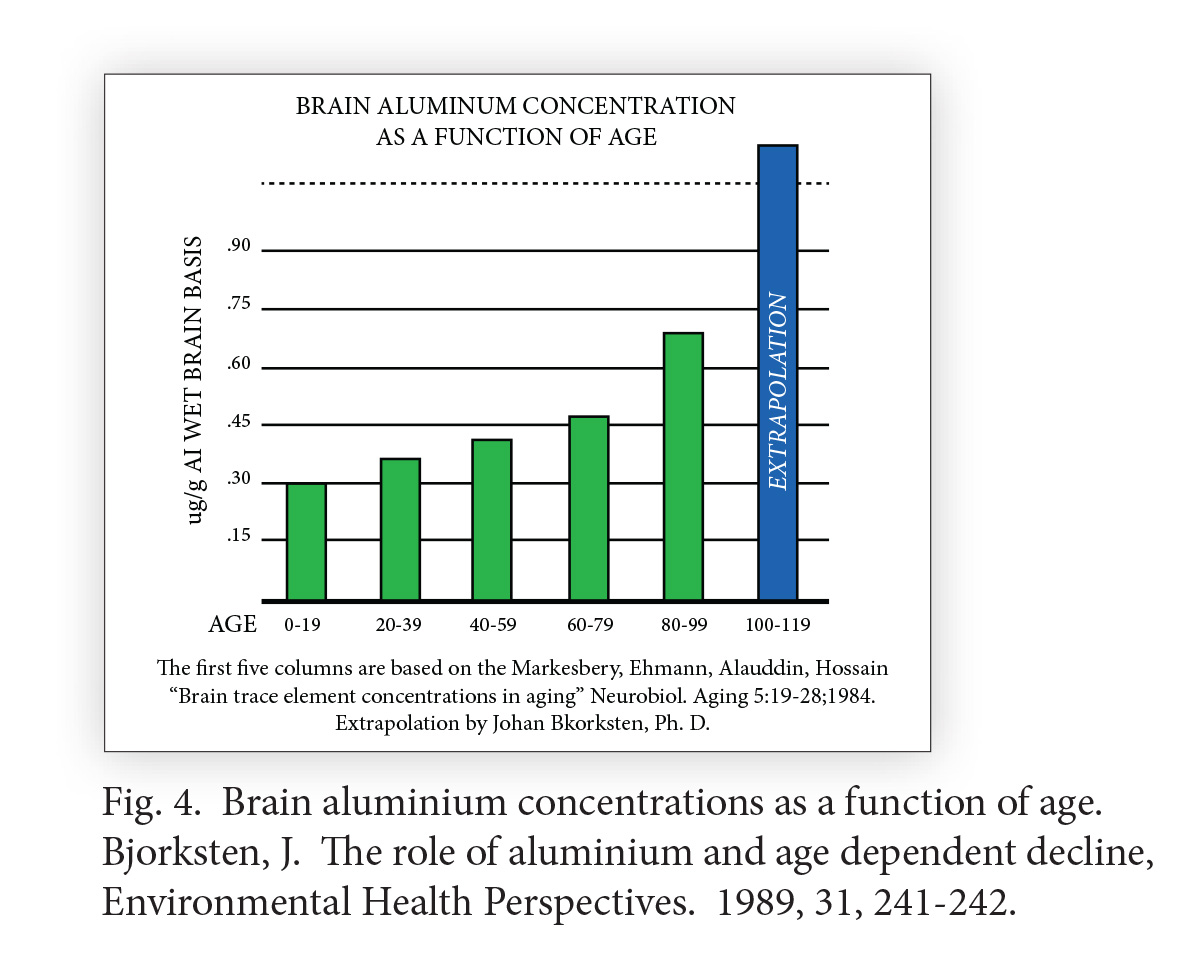
21 Bjorksten concluded that the progressive increases of aluminum with age were of great importance, and believed that the aluminum mechanism alone would limit human lifespan to 110-120 years of age even if no other cause of death intervened.22
Preventing aluminum accumulation and crosslinking
Bjorksten and his staff evaluated the ability of chelating agents to remove aluminum-containing stains from the aortas of 5-6 month-old hogs (Fig. 5).
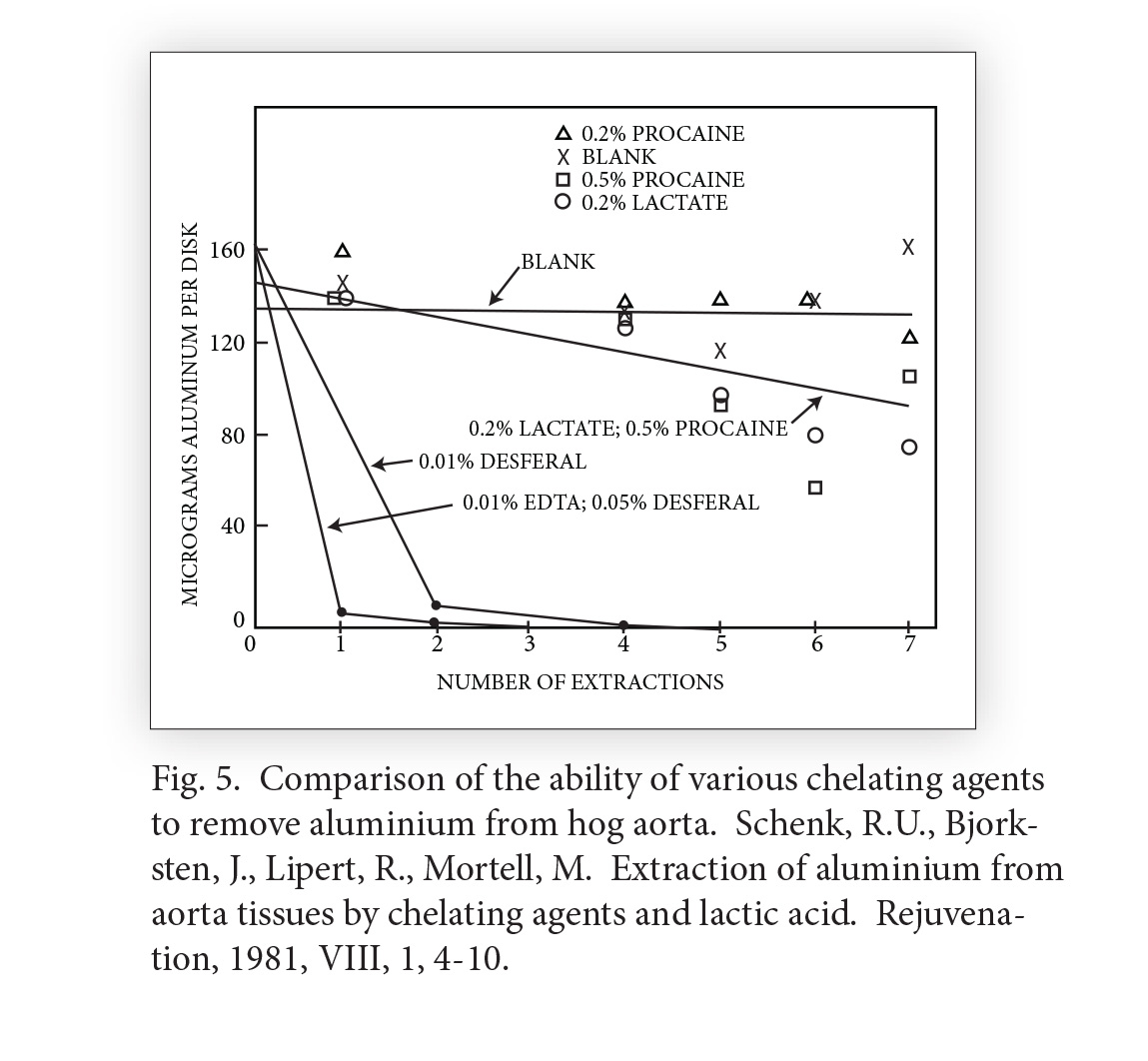
23 it can be seen that EDTA was the most effective. Lactic acid, similar to blood concentrations generated by exercise were moderately effective. Of interest was the fact that 0.5 % procaine—the active ingredient of Gerovital® (or GH3, the Romanian antiaging drug)—was also moderately effective in reducing the aluminum. This raises the question whether the metabolites of GH3—DMAE and PABA—might also have some effect in this regard.24 In fact, Drs. Imre Zs.-Nagy and Katalin Nagy demonstrated that both dimethylaminoethanol (DMAE) and centrophenoxine (CPH) are indeed able to diminish the extent of crosslinking in old rats.25
[Ed. – Original Gerovital-H3® and generic GH3-Pro® are available, as is centrophenoxine as Cent-Pro®]
Bjorksten’s team also evaluated the ability of various concentrations of lithium to remove tightly bound aluminum from tanned leather baseball covers.26, 27 Using a 0.05M concentration of lithium citrate, they completely demetalized the leather in approximately three months. Lithium is used clinically to treat manic depressive illness (MDI). Recent studies indicate that it may offer benefit in the prevention and treatment of Alzheimer’s disease, as well. 28 Perhaps long-term treatments with low doses of lithium may be an effective way to displace crosslinked/protein bound aluminum in animals and humans. Lithium orotate as a dietary supplement is the safest, most effective form of lithium available. Bjorksten spent his entire career searching for the cause and cure of crosslinks, which he believed would result in the reversal of aging and maintenance of prolonged youth. He believed that one cause of the crosslinks was heavy metal poisoning, (especially aluminum), which could be prevented and reversed with chelation therapy. He also identified the loss of fluidity of cell membranes as a contributing factor, and supported the use of membrane fluidizers such as centrophenoxine, phosphatidylserine, choline and lecithin.
Advanced Glycation End Products of Aging (AGEs)
In 1965, Dr. H.B. Bensusan proposed that a process known as the Maillard reaction, (the non-enzymatic chemical reactions between proteins and carbohydrates that cause cooked foods to turn brown) was what caused all long-lived proteins in the body to turn brown and become fluorescent, (under UV light), become more cross-linked, less soluble, less elastic, and less digestible by enzymes. In 1985, Monnier, Kohn and Cerami provided further details of the role of the Maillard reaction,1 and further developed the idea that the Maillard reaction causes premature aging and degenerative diseases such as diabetes and heart disease.29 In this regard, many scientists think the human body may be viewed as a ‘low temperature oven’ with a relatively long—approximately 75 year —‘cooking cycle.’30 The Maillard reaction involves a chemical reaction between a sugar with a protein, into a complex known as a Schiff base. With continued exposure to the sugar, the Schiff base undergoes a ‘rearrangement’ known as non-enzymatic glycosylation that results in a more stable, less reversible substance, known as an Amadori product. In the human body, this process reaches equilibrium over several weeks (Fig. 6).
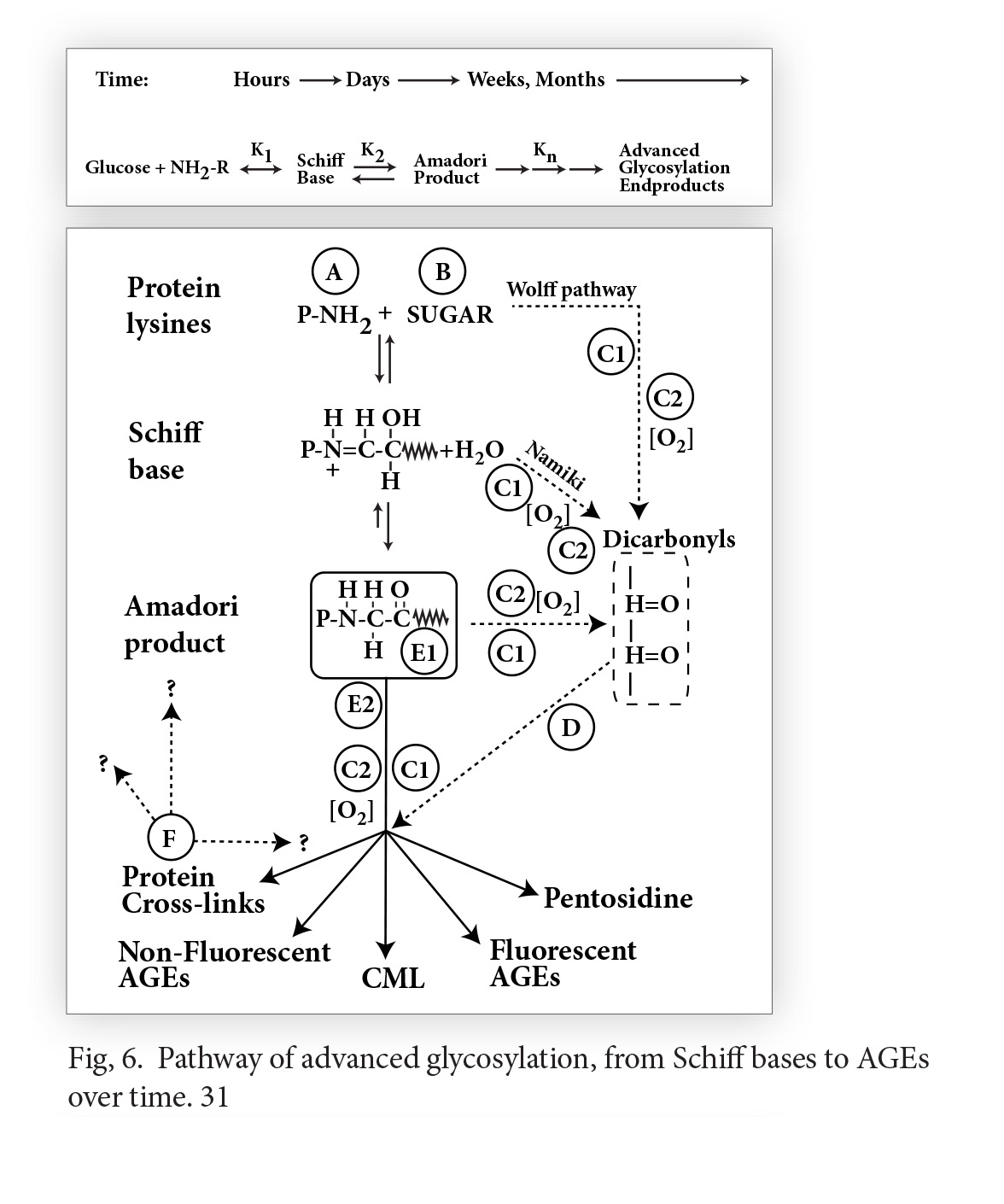
31 The Amadori product further degrades irreversibly into a number of highly reactive carbonyl (C=O) compounds called Advanced Glycation End products, designated by the acronym AGE.32 AGE is a clever pun which reflects the proposed relationship of these reactive substances to aging and age-related diseases. AGEs can further react with other fats, proteins and nucleic acids to form largely indissoluble crosslinks. The age-related accumulation of these AGE products has been demonstrated in many tissues of the body (Fig. 7).
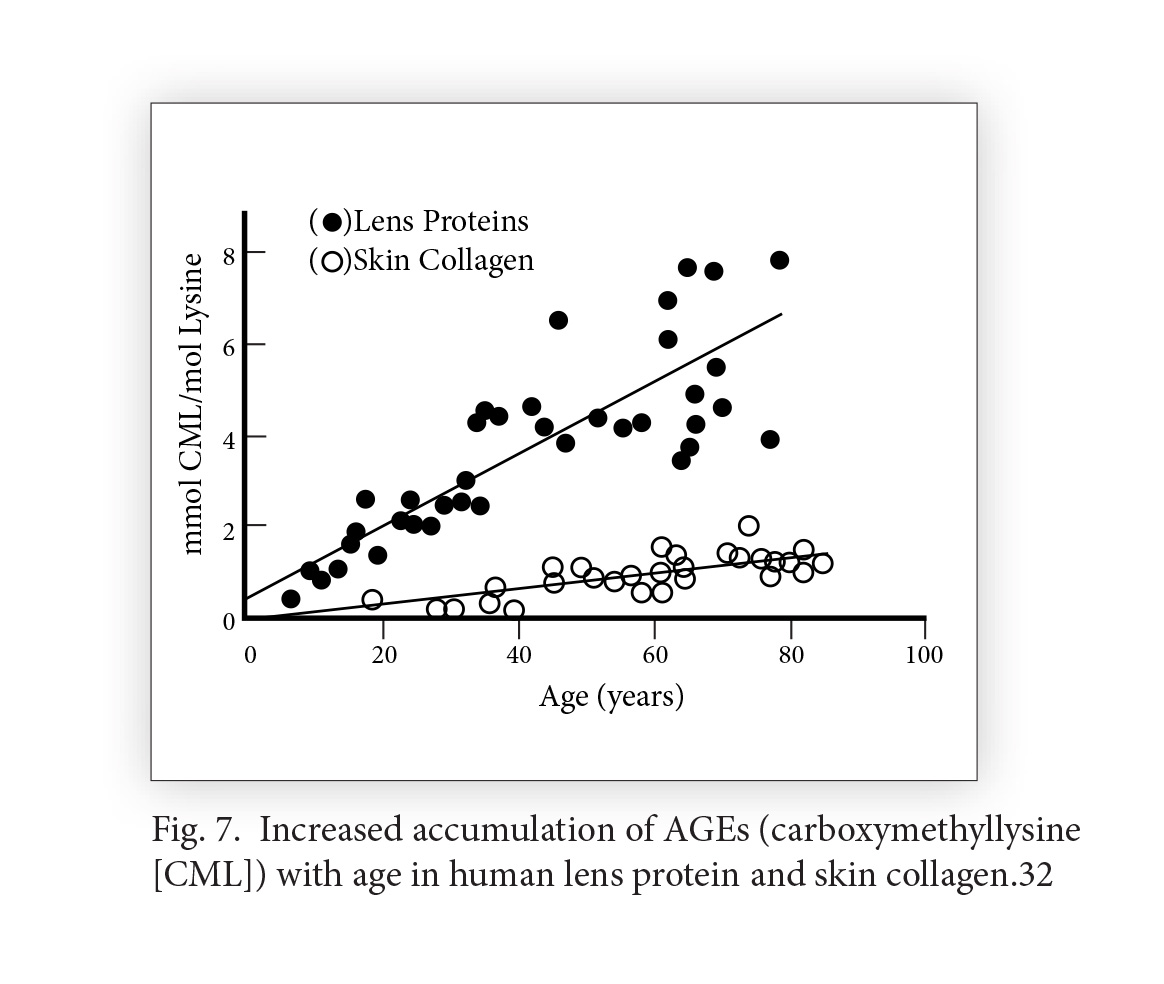
33 During long-term hyperglycemia (elevated blood sugar), as in diabetics, glycation and AGE formation may be quadrupled! This explains why diabetics suffer the premature onset of a wide range of age-related complications including cataracts, retinopathy, neuropathy, nephropathy, atherosclerosis and osteoporosis.34, 35
Crosslinkage Theory Gets New Life
Bjorksten was a talented petroleum chemist. Had he been a food chemist instead, he may have appreciated this link between the Maillard Reaction and crosslinking much earlier, and made even greater progress in developing preventive and therapeutic approaches to crosslinkage-induced aging. Through their insightful work in understanding this process, scientists like Brownlee, Cerami and Monnier provided renewed impetus and a ‘rebirth’ for the crosslinkage theory. Unfortunately, they did this with little attribution to Bjorksten, who had doggedly pursued this approach to aging for over 50 years.
AGE Breakers (and inhibitors)
There are a number of substances that have been used to delay and reverse glycation-induced crosslinkages (AGEs). Khalifah and his colleagues proposed a schematic of the formation of AGEs, and illustrates a number of specific therapeutic targets (Fig.8).31
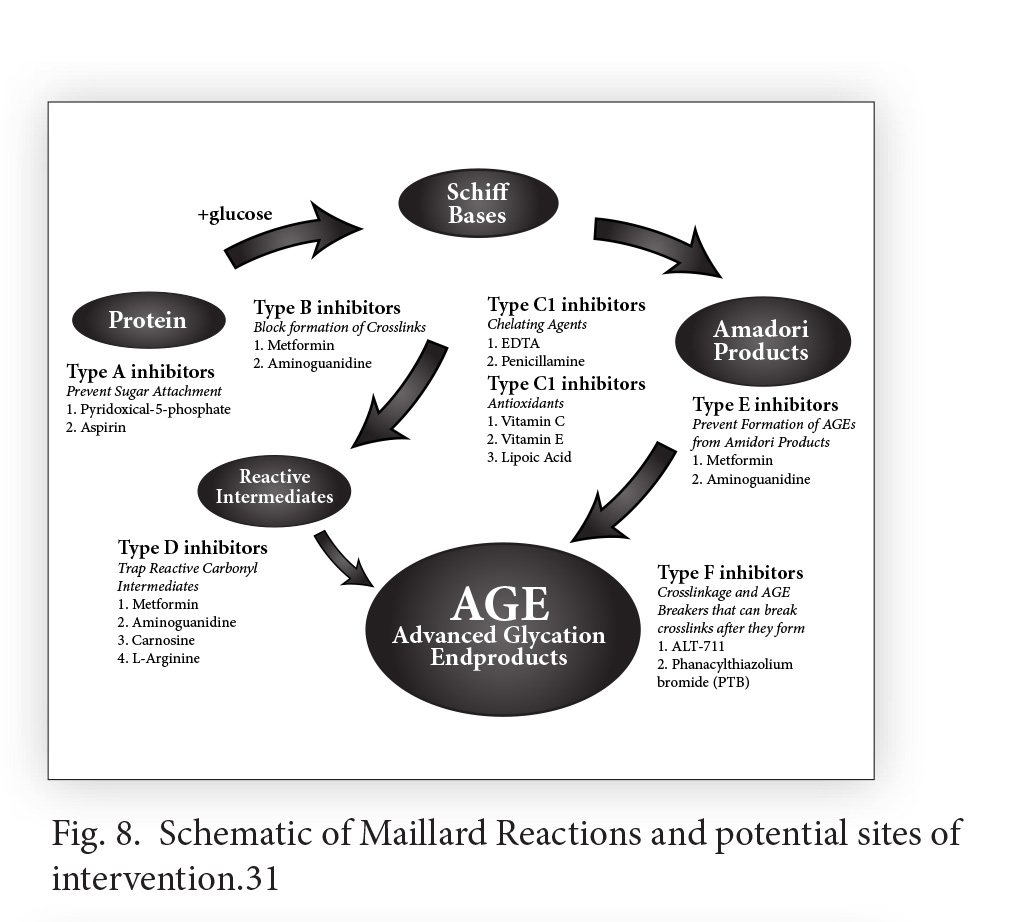
Metformin: Metformin is an anti-diabetic biguanide that was derived from the herb, Goat’s rue (Galega officinalis). Biguanide drugs were recognized by Prof. Vladimir Dilman as early as the mid-1970s as the most effective antiaging drugs in existence. Metformin is an insulin receptor sensitizer, capable primarily of lowering blood sugar and insulin. Dilman also demonstrated that biguanides restored cortisol receptor sensitivity. Metformin has many other beneficial properties, including optimizing lipid profile, reducing body fat, maintaining levels of growth hormone, stimulating immunity, and extending the maximum lifespan of experimental animals.36
Aminoguanidine (Pimegedine): Aminoguanidine is a substance that has been known for over 100 years. It is structurally very similar to guanidine, the active ingredient in the herb, Goat’s rue (the herbal prototype for metformin). Aminoguanidine has aroused a great deal of interest in the last twenty years, due to its demonstrated ability to block the formation of AGEs and AGE-induced crosslinkages in both animal and human clinical studies. Aminoguanidine inhibits AGE formation, preventing AGE-induced crosslinks in collagen and other tissues. Fortunately, aminoguanidine does not interfere with the formation of normal collagen crosslinks, which are required for structural integrity. Another mechanism by which aminoguanidine is believed to act is by enhancing the action of nitric oxide (the same mechanism by which Viagra functions).37, 38 Aminoguanidine also reduces the formation of lipofuscin (age pigment) and prevents or reduces cataracts, atherosclerosis, diabetic retinopathy, nephropathy and neuropathy (Fig. 9).
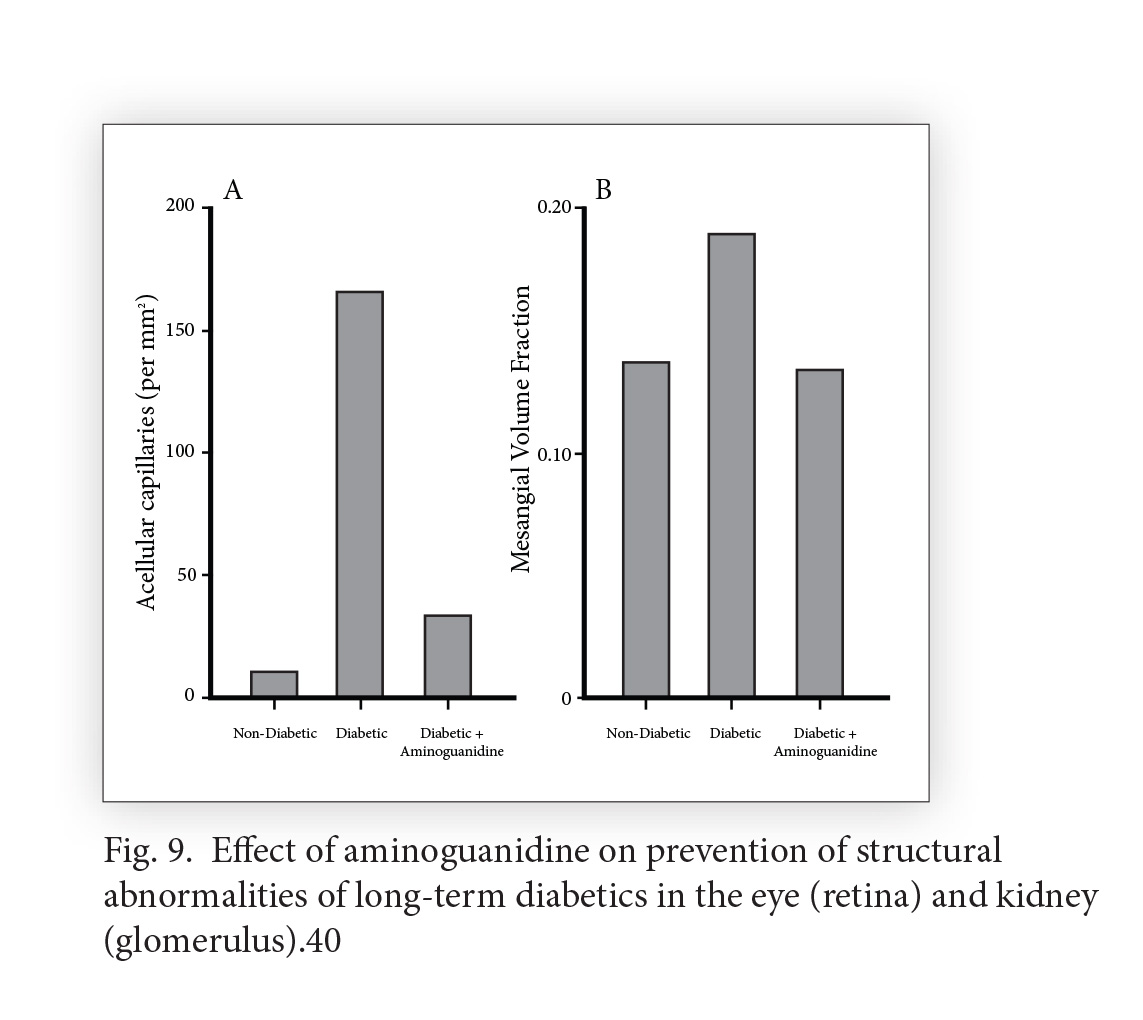
30, 39-41 In a study of diabetic patients, after four weeks of therapy with aminoguanidine, LDL cholesterol decreased almost 30%, and total cholesterol and triglycerides both decreased almost 20%. Hemoglobin-AGE levels, a circulating marker of the degree of glycosylation, also decreased dramatically (13.8 U/mg Hb at the beginning of therapy, to 10.0 U/mg Hb after only four weeks).42 Aminoguanidine is very safe, as indicated by short-term human studies which used the astronomical dose of 1200 mg daily.43 (This is in comparison with a usual human dose of 100-300 mg daily). The dose required to cause death in half the animals (mice) to which it was administered (Lethal Dose 50 [LD50]) was 1800 mg/kg.37 That would be equivalent to a human dose of almost 300 grams!
Pyridoxal-5-Phosphate (P5P): P5P, the active form of vitamin B6, has been found to significantly reduce the non-enzymatic glycosylation (formation of AGEs) of bovine serum albumin (BSA) with radioactive-labeled sugar. Of the substances tested, P5P was exceeded only by aminoguanidine in its ability to inhibit AGE formation (Fig. 10).
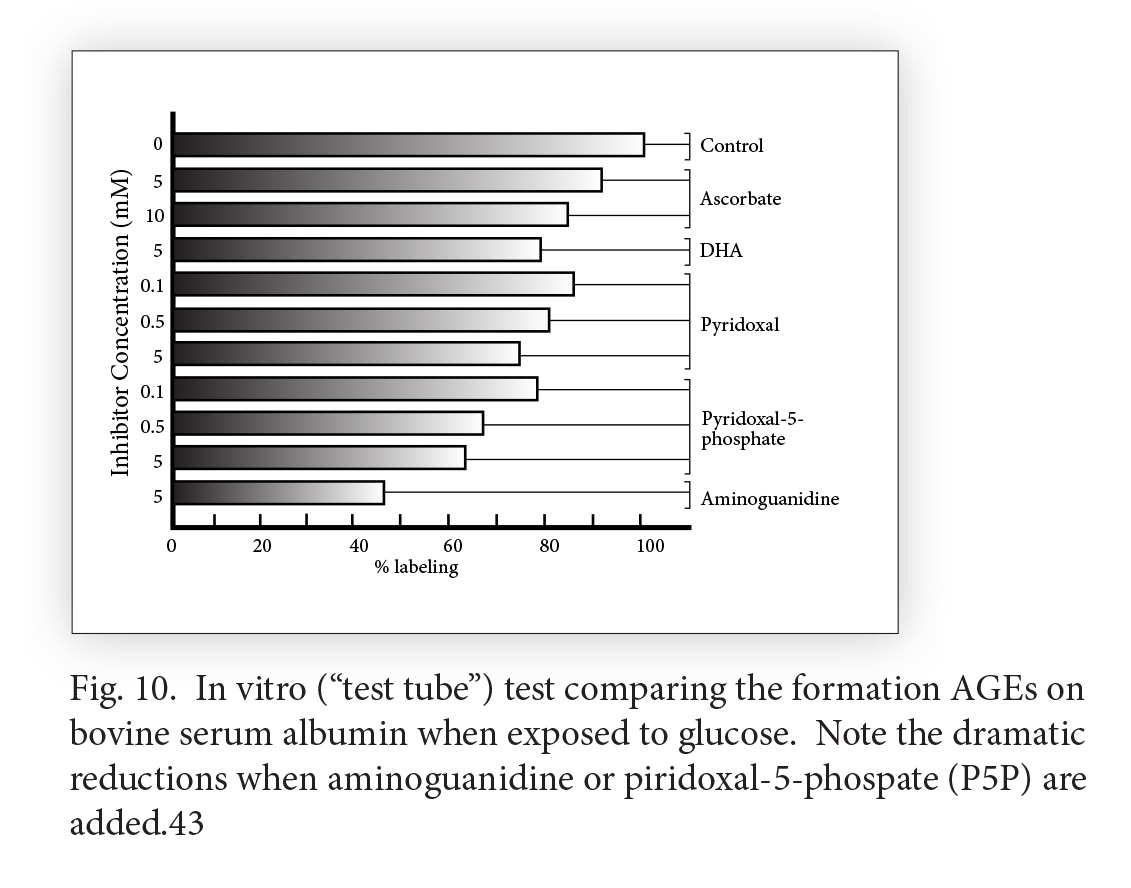
Combining P5P with metformin or aminoguanidine may enhance their AGE-inhibiting actions even more.44
Vitamin B1 (Thiamine) and Benfotiamine: In their book, Life Extension, Durk Pearson and Sandy Shaw reported that thiamine was an effective crosslink inhibitor.45 They were at that time consuming two grams of thiamine each day in their personal antiaging regimens. Thiamine may ultimately also prove to be an effective crosslinkage breaker as well as inhibitor. Another thiamine derivative is the fat-soluble Benfotiamine. Benfotiamine is very helpful in the treatment of diabetic neuropathy at a dose of 300 mg twice daily.
Carnosine: Dr. Alan Hipkiss of the Division of Biomolecular Sciences, King’s College London, reviewed the antiaging effects of carnosine and aminoguanidine.46 Dr. Hipkiss believes that one of the major mechanisms of the antiaging effects of carnosine is its powerful effects as a crosslink inhibitor and breaker, and that the use of these substances might help to control age-related molecular dysfunction. Carnosine has been used in doses generally ranging from 500-2,000 mg/day.
Sorry for this long answer to your short question—but I believe that Dr. Bjorksten’s often overlooked contributions to the glycation/crosslinking theory need to be remembered and reemphasized.
Ward Dean, M.D.
References:
- Bjorksten, Johan. Recent developments in protein chemistry, Chem Industries, 1941,48: 746-751.
- Bjorksten, Johan, and Champion, William J. Mechanical influence upon tanning, J American Chemical Society, 1942, 64: 868-869.
- Bjorksten, Johan. A common molecular basis for the aging syndrome. J American Geriatrics Society, 1958, 6: 740-747.
- Bjorksten, Johan, and Andrews, Fred. Fundamentals of aging: A comparison of the mortality curve for humans with a viscosity curve of gelatin during the cross-linking reaction. J American Geriatrics Society, 1960, 8: 632-637.
- Bjorksten, Johan. Pathways to the decisive extension of the human specific lifespan, J American Geriatrics Soc., 1977 a, 25: 396-399.
- Chappell, L.T., Stahl, J.P., and Evans, R. EDTA Chelation treatment for vascular disease: A Meta-Analysis using unpublished data. J Adv. Med, 1994,
- 3, 131-142. 7. Lau, B. Garlic for Health, 1988, Lotus Light Publications, P.O. Box 2, Wilmot, Wisconsin 53192, pp. 31-32.
- Wilkinson, S. Mercury removal by immobilized algae in batch culture systems, J Applied Phycology, 1990, 2: 223-230.
- Yaeger, Luther L., and Bjorksten, Johan. Displacement of protein bound aluminum. Rejuvenation, 1984, 12: 12-14.
- Tyler, A. Longevity of gametes: Histocompatibility, gene loss and neoplasia, in: Aging and Levels of Biochemical Organization, by Bruder, A.M., and Sacher, G.A. (eds), Section II, Part 11, 1965, U Chicago Press, Chicago, 50-86.
- Tyler, A. Prolongation of life-span of sea urchin spermatozoa and improvement of the fertilization-reaction by treatment of spermatozoa and eggs with metal-chelating agents (amino acids, versene, DEDTC, Oxine, Cupron). Biol Bull, 1953, 104: 224.
- Sincock, A.M. Calcium and aging in the rotifer Mytilina brevispina var redunca. J Gerontology, 1974, 29, 514-517.
- Sincock, A.M. Life extension in the rotifer Mytilina brevispina var redunca by the application of chelating agents. J Gerontol, 1975, 30: 289.
- Neigauz, B.M., and Ravin, V.K. Effect of physiologically active substances on the longevity of the nematode Caenorhabditis elegans. Zh. Obshch Biol, 1983, 44: 6, 835-841.
- Komarov, L.V., and Bakaev, V.V. Means of the Life Prolongation, Rejuvenation, 1983, XI: 2-3, 46-51.
- Spira, L. Clinical Aspects of Chronic Poisoning by Aluminum and its Alloys, 1933, Bale and Sons, London.
- Galle, P. , and Duckett, S. X-ray microanalysis of pallidal arteries in Parkinson Disease, Sixth European Congress on Electron Microscopy, 1976, Jerusalem, 210-211.
- Crapper, D.R., Kalrik, S., and DeBoni, U. Aluminum and other metals in senile (Alzheimer) dementia, in: Alzheimer’s Disease: Senile Dementia and Related Disorders, by Katzman, R., Terry, R.D., and Bick, K.L. (eds), 1978, Raven Press, New York.
- Crapper DR, Krishnan SS, Quittkat S. Aluminium, neurofibrillary degeneration and Alzheimer’s disease. Brain. 1976 Mar; 99(1):67-80.
- Zinsser, H., Bjorksten, I., Bruck, E.M., Baker, R.F., et al. The freezing pool: A unified sequence of the aging process, in: Medical and Clinical Aspects of Aging, by Blumenthal, H. T. (ed.), in: Proc 5th Int Assn Gerontology, 1962, Columbia U Press, 1962, 482-505.
- Markesbery, W.R., Ehmann, W.D., Alauddin, M., and Nossain, T.I.M. Brain element concentrations in aging. Neurobiology of Aging, 1984,5: 19-28.
- Bjorksten, Johan, Yaeger, Luther L., and Wallace, Terri. Control of aluminum ingestion and its relation to longevity. Internat J Vit Nutr Res, 1988, 58: 462-465.
- Schenk, Roy U., Bjorksten, Johan, Lipert, Robert, and Mortell, Molly. Extraction of aluminum from aorta tissues by chelating agents and lactic acid. Rejuvenation, 1981, 9: 4-10.
- Dean, W. DMAE and PABA — An alternative to Gerovital (GH3), the ‘Romanian Youth Drug,’ Vitamin Research News, 2001, 15: 9, 1-7.
- Zs.-Nagy, I., and Nagy, K. On the role of cross-linking of cellular proteins in aging. Mech Aging Dev, 14: 245-251, 1980.
- Yaeger, Luther L. Electrolytic scission of hexadentate aluminum bonds. Rejuvenation, 1983, 11: 76-80.
- Yaeger, Luther L., and Bjorksten, Johan. Displacement of protein bound aluminum. Rejuvenation, 1984, 12: 12-14.
- Fugate, L. Potential Role for Lithium in Preventing Alzheimer’s disease. Vitamin Research News, 2002, 16: 2, 1-7.
- Monnier, V.M., Kohn, R.P., Cerami, A. Proc. Natl. Acad. Sci., 1984, 81: 583-587.
- Dyer, D.G., Blackledge, J.A., Katz, B.M., Hull, C.J., Adkisson, H.D., Thorpe, S.R., Lyons, T.J., and Baynes, J.W. The Maillard reaction in vivo. Z. Emahrungswiss-enschaft, 1991, 30: 29-45.
- Khalifah, R.G., Baynes, J.W., and Hudson, B.G. Amadorins: Novel post-Amadori inhibitors of Advanced Glycation Reactions. Biochem. and Biophys. Res Comm., 1999, 257, 251-258.
- Brownlee, M., Cerami, A., Vlassara, H. Advanced glycosylation end products in tissue and the biochemical basis of diabetic complications. N. Engl. J Med, 1988, 318: 1315-1321.
- Cohen, M., and Van, Y. Age-related changes in non-enzymatic glycosylation of human basement membranes, Exp. Gerontol., 1983 , 18: 6, 461-468.
- Vlassara, H. Advanced glycation end-products and atherosclerosis. Annals of Medicine, 1996, 28: 419-426.
- Van Boekel, The role of glycation in aging and diabetes mellitus. Molecular Biology Reports, 1991, 15: 57-64.
- Dean, W. Aging Matters,
- Brownlee, M. Non-enzymatic glycosylation of macromolecules—Prospects of pharmacologic modulation, Diabetes, 1992, 41: Suppl. 2, 57-60.
- Friedman, E.A. Advanced glycosylated end products and hyperglycemia in the pathogenesis of diabetic complications. Diabetes Care, 1999, 22: Supplement 2, B65-B71.
- Mruthint, S., Green, K., and Abraham, E. Inhibition of cataracts in moderately diabetic rats by aminoguanidine. Exp. Eye Res, 1996, 62: 505-510.
- Forbes, J., Soulis, T., Thallas, V., Panagiotopoulos, S., Long, D., Vasan, et al. Reno-protective effects of a novel inhibitor of advanced glycation. Diabetalogia, 2001, 44: 1, 108-114.
- Brownlee, M. Glycation products and the pathogenesis of diabetic complications, Diabetes Care, 1992, 15: 12, 1835-1843.
- Makita, Z., Vlassara, H., Rayfield, E., et al. Hemoglobin-AGE. A circulating marker of advanced glycosylation Science, 1992, 258: 651-653.
- Sell, D.R., Monnier, V.M. [pentosidine] J Biol. Chem., 1989, 264: 21597-21602.
- Khatami, M., Suldan, Z., David, I., Li, W., and Rockey, H. Inhibitory effects of pyridoxal phosphate, ascorbate and aminoguanidine on non-enzymatic glycosylation, Life Sciences, 43: 1725-1731.
- Pearson, D., and Shaw, S. Life Extension—A Practical, Scientific Approach. Warner Books, New York, 1983.
- Hipkiss, A., Brownson, C. A possible new role for the antiaging peptide. , 2000, 57(5): 747-53.
- Dean, W. Carnosine: Multipurpose Anti-Aging Nutrient. Vitamin Research News, 2004, 18(9), 1-12.
Dear Dr. Dean,
In the last issue of AGING MATTERS™ Issue 3, 2013 you stated “adding a combination of potassium and magnesium for longer term use which may enable you to wean yourself form the (high blood pressure Rx) medication. I often prescribe magnesium-potassium aspartate as a source of these minerals.” My question is how much of the magnesium and the potassium? Exactly how many mgs of magnesium and potassium would be helpful for high blood pressure improvement? Thanks for any advice/suggestions.
Sincerely yours,
E.G., USA
Dear E.D.,
A good “ballpark” dose is about 5 capsules (i.e., 500 mg each of potassium and magnesium). If more is needed, I often recommend Lite Salt® as a source of potassium (340 mg per quarter teaspoon), up to one-two teaspoons per day. For magnesium, I suggest any salt of magnesium (i.e., chloride, oxide, gluconate, citrate, etc.), and increase the dose progressively over a week or two until bowel tolerance is reached (you can’t OD on magnesium, because it will give you diarrhea in excessive doses). Then back down to whatever dose is comfortable for you (i.e., moderately loose stools). Most people are deficient in these two (magnesium and potassium) intracellular cations, resulting in muscle cramps, hypertension, diabetes and other chronic diseases. I hope this answers your questions.
Ward Dean, M.D.
Dear IAS,
I was wondering if Dr Dean can recommend anything for helping with a leaky gut? It seems to stump western doctors. Many thanks.
S.B., Oregon
Dear S.B.,
For those not familiar with the Leaky Gut syndrome–which is not a diagnosis that we learn about in medical school—it is an increasingly common symptom spectrum with a constellation of symptoms such as bloating, gas, cramps, food sensitivities, chronic diarrhea and constipation, skin rashes, headaches, brain fog, memory loss, cravings for sugar and carbs, anxiety, and joint and muscle aches and pains. It is thought to be caused by a hyperpermeable (“leaky”) intestinal lining that allows larger, undigested food molecules, yeast, toxins, casein protein from milk, or other proteins in nuts, grains, or eggs, and chemicals normally found in foods (such as Phenols and Glycerin) and all other forms of waste that your body normally doesn’t allow through the intestinal lining, to flow directly into your bloodstream. These “foreign substances” are absorbed into tissues throughout the body, causing inflammation, often causing the production of antibodies against these invaders, which may result in immune dysfunction (i.e., immune deficiency or autoimmune reactions).
Symptoms of Leaky Gut vary from person to person depending on the level of damage and the tissues being affected. If left un-repaired, leaky gut can lead to more severe health issues like inflammatory bowel disease (including Crohn’s disease and ulcerative colitis), arthritis, eczema, psoriasis, rosacea, acne, depression, anxiety, bipolar disorder, migraine headaches, fibromyalgia and chronic fatigue. There is a strong body of evidence pointing to leaky gut as a major cause of autoimmune diseases including Type 1 Diabetes, as well as malabsorption of vital minerals and nutrients including zinc and iron. Leaky gut has been hypothesized to be caused by:
– Poor diet: Refined sugars, processed foods, preservatives, flours, and flavorings introduce massive amounts of chemicals into the body that may be perceived as toxic. Gluten-containing grains may damage the intestinal lining.
– Chronic Stress: Chronic stress may result in a suppressed immune system. This increases overall gut inflammation leading to increased permeability of the intestinal lining.
– Inflammation: Any type of inflammation in the gut can lead to leaky gut. This can be brought on by low stomach acid (which passes undigested food into the small intestine), yeast overgrowth (Candida), bacteria overgrowth, infection, parasites and excessive environmental toxins.
Medications: Any prescription or over the counter medication can irritate the intestinal lining.
– Lack of Zinc: Zinc is a critical piece of maintaining a strong intestinal lining. A deficiency of the vitamin can lead to the mucosal lining losing strength and becoming more permeable.
– Dysbiosis: This is an imbalance between beneficial and harmful bacteria in the gut. The overuse of prescription antibiotic drugs, tap water with chlorine and fluoride, and the lack of probiotic rich foods contribute to this imbalance.
Treating Leaky Gut requires a multi-faceted approach:
– Diet Restrictions: Reduce or eliminate sugars, starches, grains and any other irritating foods- this alleviates inflammation and starves the yeast overgrowth. Reducing these irritants allows the intestinal tract to slowly return to its normal permeability, stopping the flow of foreign substances into the blood.
– Nutritional Supplements: A good broad-spectrum multi-nutrient formula, with large amounts of vitamin D, and Zinc will help the intestinal lining return to normal (assuming the irritants from the diet are removed). Small intestinal permeability is often increased in patients with Crohn’s disease. In a study at the University of Padova in Italy, scientists sought to ascertain whether zinc supplementation would improve intestinal permeability. 12 Patients with quiescent Crohn’s disease who had increased intestinal permeability received oral zinc sulfate supplements (110 mg three times a day) for 8 weeks and were followed-up for 12 months thereafter to monitor relapses. 10 patients had normal intestinal permeability and did not relapse; of the remaining two who had increased intestinal permeability, one relapsed. The scientists concluded that Zinc supplementation can resolve permeability alterations in patients with Crohn’s disease, and that improving intestinal barrier function may reduce the risk of relapse in Crohn’s disease.
– Essential fish oils have also been shown to improve the condition of the intestinal mucosal lining (omega-3’s greatly reduce inflammation, among their other benefits).
– L-glutamine supplements strengthen the lining of the small intestine, and the amino acids proline and glycine can help heal damaged cell walls.
[Ed. – take a look at Nitric-Pro™]
Aloe Vera Juice, Licorice Root and slippery elm soothe the mucus membranes that line the digestive system, acting as a bandage. Other herbs like ginger and peppermint can also be beneficial because of their anti-inflammatory properties.
Probiotics: A good probiotic with “friendly bacteria” will stop the proliferation of bad bacteria and yeast (candida), heal the gut lining, and help nutrient absorption. I recommend at least 100 billion units of probiotics daily from a high quality brand.
[Ed. – Probiotics can be found in Dr Gordon’s Organic Greens® and also Beyond Fiber®]
I am a 64 year old woman who has been recommended to take a statin to lower my cholesterol level. From my test I have been informed that I appear to have above-normal levels of triglycerides, homocysteine and CRP. I am aware that these markers are a risk for cardiovascular disease. I am rather surprised by them because I am not overweight; I do not smoke or drink much alcohol and would say that my lifestyle is quite healthy. Therefore, I am keen to learn of which supplements could help me correct matters? (By the way I have not taken that statin drug yet).
C.K., England
Dear C.K.,
I believe you are wise not to take a statin drug, and can easily normalize all of the above markers nutritionally. Niacin (nicotinic acid, vitamin B3) is the safest, cheapest, and most effective lipid lowering substance there is. It will not only lower your total cholesterol, triglycerides, and LDL cholesterol, but it raises HDL (“good” cholesterol) (something statin drugs do not do). Depending on your levels, I usually recommend doses of 500-1500 mg per day, although doses as high as 6,000 mg have been used. Niacin causes the release of histamine, which results in a harmless but bothersome “flushing reaction” of redness, itching. The reaction is temporary, and goes away with continued use. [Ed. – IAS has Xan-Pro™ the most potent form of niacin].
Another little-known way to normalize cholesterol is by supplementing with the mineral magnesium. Most people are magnesium-deficient, which I believe results in the epidemic of hyperlipidemia which we seem to be experiencing. Magnesium supplementation mirrors the benefits obtained with niacin, i.e., lowers total cholesterol, LDL, and triglycerides, and raises HDL.1 It is nearly impossible to overdose on magnesium, as an excess will cause diarrhea. Therefore, I usually advise my patients to titrate (slowly increase) their magnesium intake to “bowel tolerance,” and then decrease the dose to whatever keeps their stools comfortably loose. Those with severely impaired kidney function should not supplement with magnesium, however. [Ed. – there are a wide range of bioavailable minerals in Quinton® water].
Homocysteine is a by-product of methionine metabolism, and is a cardiovascular risk factor in itself. Homocysteine levels can be normalized by supplementation with vitamins B6 and B12, folic acid, and anhydrous betaine (trimethylglycine [TMG]) – about 5 grams per day. C-Reactive-Protein is an indicator of inflammation in the body. It can be reduced by anti-inflammatory herbs such as Turmeric and Boswellia, aspirin, niacin, and omega-3 containing fish oils.
Ward Dean, M.D
References
- Seelig, M.S., Rosanoff, A. The Magnesium Factor, Avery, New York, 2003
Dear Dr. Dean,
“Lyme’s disease seems to be both a difficult disease to diagnose and to treat. It seems hard for me to believe in this day and age that a tick can be the cause so much trouble. My doctor is not convinced that I have Lyme’s; however I appear to have many of the symptoms including fatigue, muscle and joint pain, headaches, frequent chills, and neck stiffness. My job entails being often out and about in the Canadian wilds. Can you please recommend anything that can help in this situation? (I’m a 44 year old man).
D.D., Canada
Dear D.D.,
One of the problems that you’ve already encountered is the difficulty of making a Lyme diagnosis. The spirochete that originally causes the disease may exist in several forms, and literally “hides” within the immune system. Although there is no universally accepted test for chronic Lyme disease, I often use the Lyme Immune Tolerance Test (LITT) from Pharmasan Labs. The LITT measures the body’s cell mediated immune response to B burgdorferi-specific antigens. The diagnosis of Lyme disease remains a clinical diagnosis—i.e., a combination of the history of the illness (especially, a known tick bite), and the presenting signs and symptoms. Therefore, try to find a physician who specializes in (or is at least knowledgeable about) the diagnosis and treatment of chronic Lyme. Treatment is often frustrating, with patients responding better to one or another treatment protocol than another patient with similar symptoms. One of the best books that I have found for Lyme diagnosis and treatment is The Lyme Disease Solution, by Dr. Kenneth Singleton, M.D.—himself a long-time sufferer of Chronic Lyme Disease.
The first approach to treatment is one or more courses of antibiotics, with varying degrees of effectiveness. I have found, in addition, that oral and intravenous mild silver protein to be effective—often in combination with the immune-balancing effects of low dose Naltrexone (4.5 mg at bedtime) and baker’s yeast-derived 1-3, 1-6 Beta-glucans. Beta glucans have been shown to prime and enhance the effectiveness of the immune system in all species tested to date, including humans. The increased resistance to infection is not pathogen-specific, and extends from weaponized anthrax to flu viruses.1 Beta glucans (like naltrexone) can be used in conjunction with antibiotics, significantly enhancing their effectiveness against antibiotic-resistant bacteria. 1
In his article in Current Aging Science, a portion of which was reproduced in the first issue of this journal, Professor Paul Clayton alerted us to the enzyme lactoperoxidase (LPO) and hypo-thiocyanate (HOSCN).2 LPO and HOSCN seem to enable our immune systems to overcome virtually every pathogenic micro-organism (bacteria and viruses) against which they have been tested. Nevertheless, these substances are virtually non-toxic to humans or pro-biotics—making them a near-perfect antibiotic system.
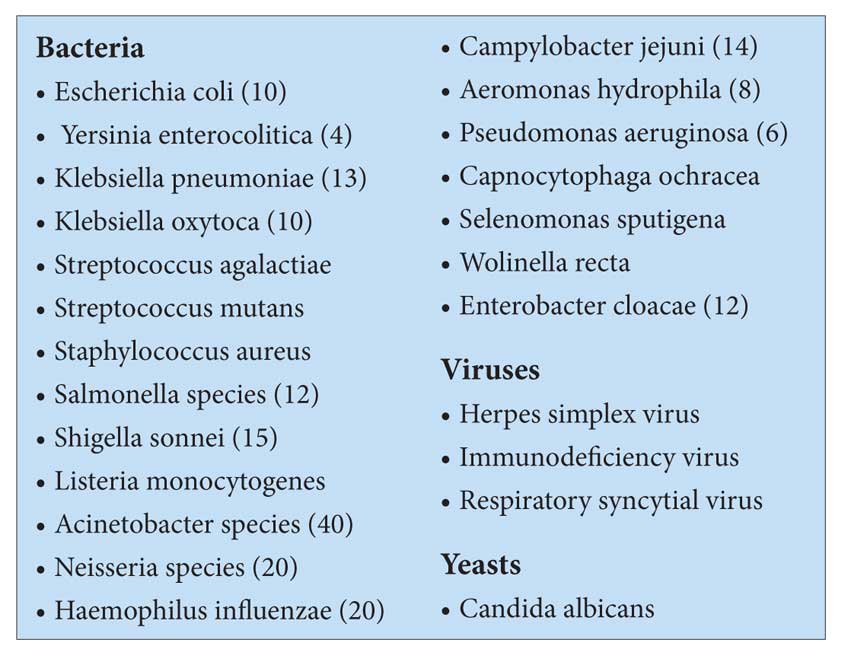
IAS offers this remarkable new approach to overcoming just about any infectious organism, in its lactoperoxidase/hypo-thiocyanate product, 1st Line™. I believe it may be equally efficacious in helping to eliminate the Lyme-causing bacteria. The microbiology and biochemistry involved in the mechanisms of 1st Line’s effects are too complex to address here, but are described in detail in Professor Clayton’s articles available on the IAS website. I hope this information will be helpful to you.
Ward Dean, M.D.
References
- 1. Clayton, P. Novel therapeutic strategies in infection and cancer management. Current Aging Science, 2012, 5, 218-224.
- 2. Clayton, P. The age of antibiotics may be coming to an end—what can we turn to? Aging Matters, 2012, 1, 21-23.
Dear Dr. Dean,
I am a type I diabetic patient, on an insulin pump. I also take 1,500 mg of Extended Release Metformin each day. I suffer from obesity, and am trying to lower my HbA1c to a 6. I am enclosing my personal report from my physician for the past 5 years. Can you give me any suggestions? Thank you,
D.N.A., Dubai
Dear D.N.A.
Thanks for sending your lab work and the note from your physician. First, I think you should increase your dose of Metformin to 1,000 mg twice daily.
Next, I recommend you add several other anti-diabetic medications to your regimen. Acarbose (available from IAS) is a “starch blocker.” It slows the conversion (digestion) of complex carbohydrates like bread, pasta, rice, beans and starchy vegetables into simple carbohydrates (sugar). I suggest chewing one 100 mg Acarbose tablet with each starchy meal. The most common side effect is intestinal gas—which is not caused by Acarbose, but by the undigested food fermenting in the intestines. This is a signal that Acarbose is doing its job, and you are eating the wrong foods. But it provides you with a “cushion” for your diet. Incidentally, Acarbose is the most widely used anti-diabetic drug in China.(1) I incorporate Acarbose into the weight-loss programs of many of my patients.
Another class of anti-diabetic drugs to consider is the DPP-4 inhibitors, such as Onglyza, Tradjenta, or Januvia. Discuss these with your physician, and see if he will prescribe one for you. DPP-4 inhibitors work well with Metformin, and further help restore insulin receptor sensitivity. These drugs also help regenerate pancreatic beta cells, to help your body produce its own insulin. They are all generally useful adjuncts for weight loss.
Yet another class of medications you might add is Victoza—the glucagon-like peptide-1 (GLP-1) agonist Victoza (liraglutide). This drug is injected (like insulin), but unlike insulin, will not cause hypoglycemia. Victoza appears to be even more effective than the DPP-4 inhibitors for helping with weight loss. None of the drugs that I suggested above will cause hypoglycemia. They all act by different and complementary mechanisms to normalize your blood sugar, and will enable your insulin to work more efficiently. Your requirement for insulin will be decreased, and you will most likely need to reduce your dosage. That will be beneficial for weight loss, as insulin is the hormone that drives blood sugar into the cells, where it is stored as fat. Hopefully, you will be able to eliminate the insulin entirely.
In addition to controlling your diabetes, I think it is very important for you to correct your abysmally low level of Vitamin D. IAS has a convenient, once/week capsule that contains 50,000 IU of Vitamin D-3.
I hope these suggestions will be helpful for you. Sincerely,
Ward Dean, M.D.
References:
1. Alpha-glucosidase inhibitors 2012—cardiovascular considerations and trial evaluation. Standl, E., and Schnell, O. Diabetes & Vascular Disease Research 9(3) 163-169.
Dear Dr. Dean,
I was wondering if questions can still be forwarded to Dr Dean.I am particularly interested in what he might have to say about the recent link claimed between testosterone and heart attack, stroke, etc.I have been on a program using cypionate for replacement with wonderful results for the last ten years. I would love to hear his comments.
Thanks,
L.G., USA
Dear Mr. Guittard,
Thanks for giving me the opportunity to address this important issue
Your question is based on publicity surrounding the study in the November 6th, 2013 issue of the Journal of the American Medical Association (JAMA-1), which frighteningly concluded that “the use of testosterone therapy was associated with increased risk of adverse outcomes.”
This was a shockingly flawed study, with more holes in the data and their interpretation than a block of Swiss cheese. I am amazed that this paper was ever published–especially in such a prestigious journal.
Let me put things in perspective. The paper was a “retrospective cohort study,” conducted by a review of medical records from 76 cardiac catheterization laboratories in the VA system. The study involved the records of 8,709 men who had undergone coronary angiography between 2005-2011, who had testosterone levels less than 300 ng/dl. Of the 8,709 “participants,” 1,223 were in the “testosterone group.” This testosterone group was a hodge-podge comprised of those who had received one prescription for testosterone (17.6%) or more than one (82.4%). 13 (1.1%) of the men were treated with topical gels, 436 (35.7%) with injections, and 774 (63.3%) with patches. Of those who had received “more than one prescription,” the mean number of days from first fill to last fill of testosterone was 376 days. Of the patients in the testosterone group, 734 (60%) had a subsequent testosterone level drawn. The baseline testosterone in the treatment group was 175.5 ng/dl- -and (for the 60% who had follow-up testosterone levels checked) testosterone was increased to only 333.2 ng/dl.
The statisticians who wrote the study used “stabilized inverse probability of treatment weighting” to assess the association between testosterone therapy and the primary outcome of death, heart attack, and stroke, and used a number of variables to create these “weights,” including “comorbidities” (41 diseases) and “procedures” (13 procedures).
The authors reported in the introduction that of the 7,486 patients not receiving testosterone, 681 died, 420 had heart attacks, and 486 had strokes. Of the 1223 patients who had received testosterone, 67 died, 23 had heart attacks, and 33 had strokes.
I am not a statistician. I was never very good at math. But it is pretty easy to calculate that there were 6 times the number of patients in the no-treatment group compared to those who received testosterone. If we multiply the incidence of adverse outcomes in the testosterone-treated group by 6, we arrive at only 402 (6 x 67) who would have died in the treatment group (versus 681 who died in the no treatment group); 138 (6 x 23) who would have had heart attacks in the treatment group (versus 420 no treatment); and 198 (6 x 33) who would have had strokes (versus 486 no treatment).
Thus, it is a complete mystery to me how the authors, using their advanced statistical manipulations, arrived at their clearly erroneous conclusion that “the use of testosterone was associated with increased risk of mortality, MI, or ischemic stroke,” when the results plainly indicate that testosterone use resulted in a much lower percentage of adverse events. This confirms the old adage that “figures don’t lie, but liars can figure.”
The statistical anomalies are not the only flaw in this study.
Recall that to be enrolled in this study, a subject had to have undergone coronary angiography. Obviously, these men had all already been determined to be at risk for death, heart attack or stroke, (the “end points” of the study) due to their having been referred for angiography. Healthy men do not undergo coronary angiography.
The other criteria for inclusion was a testosterone level less than 300 ng/dl. A recent study in the Journal of the American College of Cardiology evaluated the relationship between testosterone levels and risk of cardiovascular (CV) events in 2,416 men aged 69-81 years, over five years.(2) The researchers found that testosterone levels were inversely associated with the risk of CV events (i.e., those with the highest testosterone had the fewest “events”). They reported that men in the highest quartile of testosterone (more than 550 ng/dl) had a lower risk of CV events compared to the men in the 3 lower quartiles (recall also that the men in the testosterone-treated group in the JAMA study raised their testosterone to only 332.2 ng/dl). The researchers concluded that “High serum testosterone predicted a reduced 5-year risk of CV events in elderly men.”
Another recent study of 1031 male veterans over age 40 with low testosterone (less than 250 ng/dl) also contradicts the JAMA study. (3) In this paper, 398 of the patients were treated with testosterone. The mortality over 5 years was 10.3% in the testosterone-treated men versus 20.7% in the untreated men. The authors reported that “testosterone treatment was associated with decreased risk of death.”
More recently, three eminent physicians reviewed the JAMA study. (4) They stated that “We have serious concerns regarding the validity of these results based on author errors, study design, data presentation, methodology, and ultimately common sense.” They examined the JAMA article point-by-point, and concluded that “We believe the evidence to date strongly suggests that testosterone therapy improves CV risk. We reject the assertion by Vigen, et al that testosterone therapy increases CV risks or mortality.”
If this is not enough to set your mind at ease, consider the other potential benefits of testosterone therapy that were curiously conceded by the authors of the JAMA study–testosterone replacement therapy improves sexual function, 5-7 bone mineral density, 8,9 increases free-fat mass 8,9 and strength, 10 improves lipid profiles 11-13 and insulin resistance, 11,12 and increases the time to ST depression during stress testing. 14,15
My only caution to those using testosterone supplementation is to monitor the CBC (to insure that the hematocrit does not rise above normal, causing “thicker” blood) and estrogen levels (testosterone aromatizes into estrogen, which can be controlled with low doses of anastrozole) and to maintain the testosterone level in the “safe” range, i.e., above 550 ng/dl.
Ward Dean, M.D.
References;
- Vigen R, O’Donnell CI, Barón AE, et al. Association of testosterone therapy with mortality, myocardial infarction, and stroke in men with low testosterone levels. JAMA. 2013;310(17):1829-36.
- Ohlsson C, Barrett-Connor E, Bhasin S, et al. High serum testosterone is associated with reduced risk of cardiovascular events in elderly men. The MrOS (Osteoporotic Fractures in Men) study in Sweden. J Am Coll Cardiol. 2011 Oct 11;58(16):1674-81.
- Shores MM, Smith NL, Forsberg CW, Anawalt BD, Matsumoto AM. Testosterone treatment and mortality in men with low testosterone levels. J Clin Endocrinol Metab. 2012 Jun;97(6):2050-8. doi: 10.1210/jc.2011-2591. Epub 2012 Apr 11.
- Traish, AM, Guay, AT, and Morgenthaler, A. Death by Testosterone? We Think Not! J Sex Med, 2014; 11:624-629.
- Wang C, Swerdloff RS, Iranmanesh A, Dobs A, Snyder PJ, Cunningham G, Matsumoto AM, Weber T, Berman N; Testosterone Gel Study Group. Transdermal testosterone gel improves sexual function, mood, muscle strength, and body composition parameters in hypogonadal men. J Clin Endocrinol Metab. 2000 Aug;85(8):2839-53.
Dear Dr. Dean,
I am a 50 year old man in decent health- certainly with no medical conditions. I have never smoked, I drink alcohol rarely and do my best to eat and live well. Recently I have had some stabbing pains in my toes/ feet and occasionally in my hands. This usually occurs when I lie down to sleep. It is not debilitating, more frustrating. However if it is a prequel to some problem, I would rather deal with it now and therefore would greatly appreciate your opinion.
P.M., Ireland
Dear Mr. P.M.,
Based on the limited information provided, the problem seems to be most likely some kind of neuropathy or ‘mini-seizure.’ How long has this been going on, and is it getting worse over time? Several suggestions would be to try Benfotiamine, about 300 mg twice per day and Gabapentin (Neurontin®) at bedtime, in a dose ranging from 300-1800 mg. A third suggestion is to add Lithium Orotate (2 caps twice daily).
Benfotiamine is a fat-soluble form of vitamin B1, which has been shown to be of benefit in diabetic and peripheral neuropathy.
Neurontin® is an anti-seizure medication that is used for a number of conditions, including peripheral and diabetic neuropathy, restless legs, alleviation of menopausal hot flashes (unrelated to your condition of course), and insomnia. (1) I usually start my insomniac patients on 600 mg at bedtime, and have them titrate the dose up or down to what works for them. Neurontin® is remarkably free from side effects, (other than causing drowsiness and inducing sound, restful sleep) and does not adversely interact with other medications. (2) When properly dosed, patients experience sound, restful sleep, and awaken feeling refreshed. If you are groggy upon awakening; (at any dose) then try reducing the dose, or taking it earlier in the evening. The usual effective dose is 600-800 mg at bedtime, but some very sensitive people need only 300 mg and some require up to 1800 mg. The dose of 2400 mg per day is the usual maximum dose, although dosages as high as 3200 mg have been reportedly used.
Lithium Orotate acts as a ‘nerve stabilizer,’ and may be helpful in your situation. Lithium Orotate is 20 times more bioavailable than prescription forms of lithium and can therefore be used in fractional doses compared to the prescription forms of lithium. Because of the low doses used, blood ‘lithium levels’ are not necessary, as are required with prescription lithium. Let me know how you do.
Ward Dean, M.D.
References:
- 1. Lo HS, Yang CM, Lo HG, Lee CY, Ting H, Tzang BS. Treatment effects of gabapentin for primary insomnia. Clin Neuropharmacol. 2010 Mar-Apr;33(2):84-90.
- 2. Karam-Hage, M., BROWER, KJ. Gabapentin treatment for insomnia associated with alcohol dependence. Am J Psychiatry 2000;157:151-151.
Dear Dr. Dean,
I have just read about Lactoperoxidase (LPO) and Hypo-thiocyanate (1st Line™) through the Aging Matters™ magazine, and read the referenced papers from Professor Clayton. IAS promotes 1st Line as a remarkable new approach to overcoming just about any infectious organism. I have systemic candida & mold/ tricothecene, and am interested in taking 1st Line™, but have a few questions:
1. My doctor days that colostrum–a whole food which also contains LPO–would be preferable. What do you think?
2. How much would I take of the 1st Line product?
3. Where does 1st Line come from [i.e. what are the manufactured ingredients & source]?
4. Is it likely to combat fungus/mold?
Thank you in advance for any guidance you may be able to provide.
Regards
S.L., USA
Dear Mr. S.L.,
First, are you sure about exposure to the mold mycotoxin, tricothecene? There is no known cure for mycotoxicosis, and tricothecene is one of the most toxic, stable types of mycotoxins. With regard to your specific questions:
- Colostrum may help, but I don’t think it will replace the benefits of 1st Line™. Colostrum does contain LPO, but in very small amounts and does not deliver oxythiocynate (OCN). I don’t believe it will trigger the ion release that a kit of 1st Line™ will. 1st Line™ delivers 25 mg of oxythiocynate ions (OCN), which are on the ‘sharp end’ of destroying the infections. These ions are activated by LPO, so colostrum may enhance the efficacy of 1st Line™.
- Dosage is difficult from a distance, but considering the potential seriousness of mycotoxin exposure, I suggest 2 kits on successive days. It is not recommended to take more than a kit per day, (thus doubling the normal dose of OCNs in salvia, tears, milk etc.) Herpes patients consume a kit a day for 7-days and then a kit per month to control outbreaks. You may not need so much, but it all depends on where the mold is located, the degree of your exposure, and the state of your immune system.
- The ingredients are no secret and are located here: www.antiaging-systems.com/approveduses/14-1st-line. Specifically, they include: Hydrogen peroxide, lactoperoxidase and bentonite. The components are manufactured, matching the chemicals that are naturally found in the saliva/ tears/ milk.
- Yes, 1st Line™ will combat fungus/mold.
It is essential to reduce/eliminate your exposure to these mycotoxins. Unfortunately, there are not many ways to destroy them. One way is through fire (tough, if it is your house that is contaminated). Another way is bleach with 5% sodium hypochlorite. Sodium hypochlorite is described as MMS (Miracle Mineral Solution), and you can find excellent discussions of its therapeutic use for combating mold and mycotoxins at www.curezone.org. Ozone might also destroy some mycotoxins, and you might consider autohematogenous therapy with ozone. I hope these suggestions will help,
Ward Dean, MD
Dear Dr. Dean,
I am 41 years old. I had a borderline ovarian tumor removed 6 years ago and as a result have been on estrogen replacement because of a total hysterectomy. I had an abdominal CT recently, it shows hepatic steatosis. I drink very little alcohol, my BMI is 20.62, and my cholesterol and liver enzymes are excellent. Can fatty liver be reversed?
A. P., USA
Dear Mrs. A.P.,
Scientists from China recently reported metformin to be the treatment of choice for hepatic steatosis (fatty liver). I recommend 500 mg three times daily. (Reference: Liu, F., et al. Metformin prevents hepatic steatosis by regulating the expression of adipose differentiation-related protein. Int J Mol Med, 33: 51-58, 2014)
Ward Dean, M.D.
Dear Dr. Dean,
I’ve tried many diets over the years to lose weight, but few seem to have any lasting or significant effect on me. I am aware of the problems of carbohydrates and try to limit them, but they are one of my eating weaknesses. Please recommend something for a 40-year old woman that can aid my lifestyle changes and make it happen!
N.M., Thailand
Dear N.M.,
Overweight is one of the most common and most difficult to treat of the chronic degenerative diseases. The cause is multifactorial. It is not psychological weakness. One of the most common contributing causes is undiagnosed or undertreated sub-clinical or overt hypothyroidism. See Dr. Rick Wilkinson’s article, “The Epidemic of Low Thyroid Diseases,” in Issue # 4, 2014 of Aging Matters Magazine, for more on this important condition.
Unfortunately, if one has many hypothyroid symptoms (which may include cold hands and feet, hyperlipidemia, low energy, difficult weight loss, depression, constipation, menstrual problems) but “normal” thyroid blood tests, it will be difficult to find a physician who will prescribe an appropriate dose of thyroid.
I follow guidelines similar to those recommended by Dr. Wilkinson (and our mentor, Broda Barnes, M.D.1). If a patient has a panoply of hypothyroid symptoms (especially weight gain), I start the patient on 1 grain of Armour Thyroid, and titrate the dose up or down over several months, based on the patient’s response, body temperature, and heart rate. If the heart rate stays in the normal range (60-80), and the patient feels well, there is little likelihood of causing an overdose, regardless of the blood test results. I have generally found that thyroid function blood tests are a waste of blood.
In Aging Matters, Issue # 2, 2014, in his article “The Rotational Origin of Diseases and Aging,” Prof. Walter Pierpaoli seems to agree, where he stated, “…the laboratory assays [for thyroid] are totally misleading and wrong!” He recommended keeping TSH at ZERO and ‘free’ T3 with ‘free’ T4 two-three times higher!
A second and more common cause of overweight is hyperinsulinemia, or dysmetabolic syndrome. As we grow older, we are all turning into diabetics (or becoming “pre-diabetic”). We tend to become insulin resistant, and our pancreas compensates by producing more insulin. Insulin is the hormone that drives glucose from the blood into the cells where it is used to produce energy—and what’s left over is stored as fat. This was the basis of the Atkins Diet—a high-protein, high-fat, low-carbohydrate diet designed to minimize rises in blood glucose and insulin. Atkins knew that “carbs are the enemy.”
For my overweight patients, I routinely recommend 500 mg Metformin, taken three times per day. Metformin acts as a “metabolic rejuvenator,” restoring insulin receptor sensitivity, and delaying a process known as “hepatic gluconeogenesis,” by which the liver produces sugar from non-carbohydrate sources.
Patients taking Metformin feel better, have more energy, and lose their carbohydrate cravings—and generally lose body fat. For more information on Metformin, please see my article in Issue # 4, 2013 of Aging Matters, titled, “Metformin Update: Still the most effective anti-aging, life extension drug, with a broad range of benefits.”
Another anti-diabetic drug that I include in my weight loss program is Acarbose, an alpha-glucosidase inhibitor. Acarbose acts at the brush border of the small intestine, where carbohydrates are broken down into sugar which is then absorbed. By blocking the breakdown of most carbohydrates into sugar, post-prandial (after-meal) blood glucose levels are suppressed, and fewer calories from glucose are absorbed (Fig).
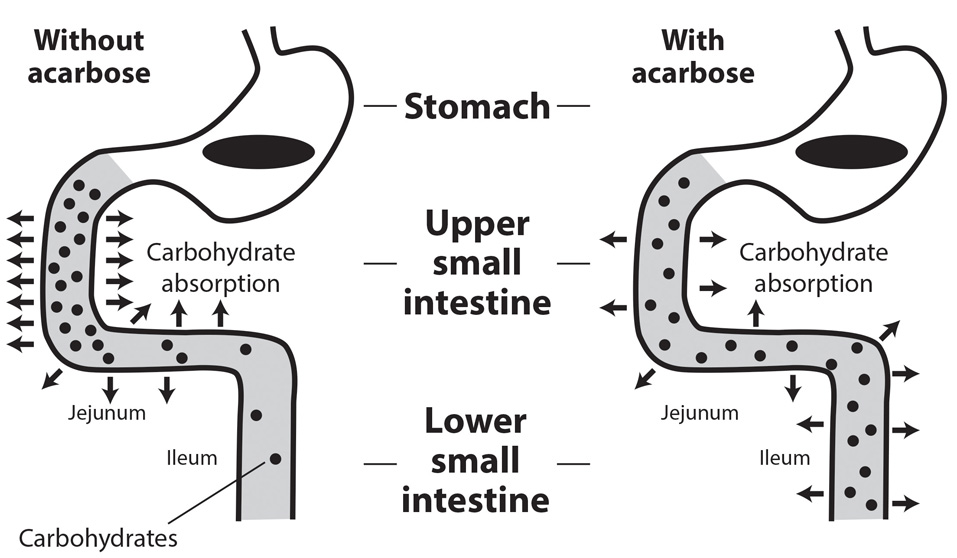
Normal carbohydrate consumption, without Acarbose, is illustrated on the left. However, when Acarbose is consumed with starchy food, less glucose is released, and less glucose is absorbed, resulting in reduced absorption of calories from starchy foods.2
The undigested carbohydrates, upon reaching the colon, may ferment, producing uncomfortable gas. This usually becomes less bothersome with continued use, but if it is unpleasant, you can reduce the dose of acarbose with each meal. Most studies of Acarbose, when used alone, do not result in significant weight loss, However, in my experience, used in combination with Metformin, Acarbose significantly enhances the weight-loss benefits of Metformin.
I think you will find the combination of an Atkins-like diet, Armour thyroid, Metformin and Acarbose will help you “turn around,” and reach your weight loss goal.
Good luck,
Ward Dean, MD
References:
1. Barnes, B., and Galton, L. Hypothyroidism: The Unsuspected Illness. Harper & Row, New York, 1976.
2. Standl, E., and Schnell, O. Alpha-glucosidase inhibitors 2012—Cardiovascular considerations and trial evaluation. Diabetes & Vascular Disease Research 9(3) 163-169.
I’ve read a lot of your stuff over the years and know that you’re a big fan of niacin (Vitamin B3, nicotinic acid) for normalizing blood lipids. What are your thoughts regarding the recent study in the New England Journal of Medicine, which disparaged the lipid-lowering benefits of niacin and implied that it was actually toxic?
Dear Mr. J.E.,
Thanks for giving me the opportunity to respond to this issue. The study in question was not a study of niacin, per se. It was actually a study comparing the addition of extended-release niacin plus laropiprant, (an antihistamine which purportedly reduced niacin-induced flushing) to patients who were already taking simvastatin 40 mg per day, or simvastatin plus ezetimibe 10 mg per day, (ezetimibe is a drug that is designed to increase HDL). (1)
I was really surprised to note that it wasn’t just a single article warning against niacin. The same issue of the New England Journal coincidentally had a Letter to the Editor, questioning the “Safety Profile of Extended-Release Niacin in the AIM-HIGH Trial,” (2) and an Editorial, “Niacin and HDL Cholesterol—Time to Face Facts” (3)—i.e., a triple take-out piece!
The study involved 25,637 high-risk patients from 245 test sites in the UK, Scandinavia, and China. The “placebo” group received Simvastatin 40 mg or Simvastatin 40 mg plus Ezetimibe 10 mg, plus a 50 mg low-dose niacin-containing “placebo.” The “niacin” group received 2,000 mg of extended-release niacin and 40 mg of Laropiprant, in addition to the Simvastatin or Simvastatin plus Ezetimibe, as was given to the placebo group. The participants in the study were followed for a median of nearly four years. The study was stopped prematurely after three years because of an apparent lack of benefit with extended-release niacin (plus laropiprant).
The authors concluded that the Niacin-Laropiprant combination; “did not significantly reduce the risk of major vascular events, but did significantly increase the risk of serious adverse harm,” and alleged that, “the study identified significant hazards, some of which had not been reported previously with niacin.”
Let’s digress. The cholesterol-lowering effects of nicotinic acid were first reported in 1955.(4) The clinical benefits of immediate-release nicotinic acid were best demonstrated in the Coronary Drug Project (CDP), which compared immediate-release niacin with other cholesterol-lowering regimens on cardiovascular end points.(5) In the CDP, immediate-release niacin reduced the total cholesterol level by 26 mg/dl (from a high baseline level of 253 mg/dl) and after six years, reduced the incidence of non-fatal MI (heart attacks) by 26% and cerebrovascular events (strokes) by 24%. Moreover, 9 years after trial termination, the group treated with niacin had 11% fewer deaths than the placebo group (Fig. 1). (5) Although lipid fractions were not measured in the CDP, subsequent studies with immediate-release niacin showed that it reduces LDL up to 25%, triglycerides up to 50% and Lp(a) up to 35%; and increases HDL up to 35%. (6-8)
The most commonly reported side effect of immediate-release niacin are the well-known flushing and itching of the skin, (cutaneous vasodilation) that can be so uncomfortable that it may cause some people to discontinue taking it. Although the flushing can be overcome by taking niacin at the end of a meal, or by taking an aspirin 30 minutes prior to taking niacin, it is also self-limited and tolerance to flushing develops with continued use. Nevertheless, pharmaceutical companies developed timed-release preparations to minimize or eliminate this effect. Unfortunately, timed-release niacin is less effective (and more toxic) than immediate release, cheap, over-the-counter niacin (Fig. 2).
Now back to the New England Journal study. The “serious adverse harm” included “diabetes-related, gastrointestinal, musculoskeletal and skin-related disorders,” which the authors stated were previously known to be caused by niacin. Additionally, the authors stated that most of the serious musculoskeletal adverse events with niacin-laropiprant were due to myopathy, (muscle weakness, pain and atrophy); and there was an unexpected finding of excess serious infection and serious bleeding events. The authors further claimed that “niacin alone” was also associated with a significant increase in the risk of serious infection in a previous study as well (AIM-HIGH10). (1)
The AIM-HIGH study, 10 however, was not a study of “niacin alone”—it was a study that also combined extended-release niacin with intensive statin therapy.
With regard to the excess bleeding, the authors conceded that it may not have been due to niacin—but may have been due to laropiprant – as several potential mechanisms for bleeding have been previously proposed for laropiprant, (11,12) and niacin has not previously been reported to cause bleeding problems.
The authors of the New England Journal study curiously overlooked the fact that the FDA in 2012 required that labels on statin drugs be changed to include information concerning statin-induced glycemic effects, diabetes and increases in hemoglobin A1C or fasting plasma glucose. (13) This label change was based on several meta-analyses that demonstrated the relationship between statin use and diabetes. One meta-analysis examined the effect of statins on the risk of diabetes in 91, 140 patients from 13 trials, which showed that statins were associated with a 9% increased risk of diabetes. (14) Another meta-analysis of 32,752 patients, in five trials, found that higher potency statins were associated with a 12% increased risk of diabetes, compared to low potency statins. (15) Simvastatin, at a dose of 40 mg (as used in the New England Journal study), was considered to be a high potency statin. (16)
Although immediate-release niacin may cause reductions in glucose tolerance when treatment is initially begun, studies show that glucose generally returns to pre-treatment levels with continued use (17, 18)- (Fig. 3). On the other hand, the package insert for extended-release niacin, (as used in the New England Journal study) cautions that “NIASPAN can cause an increase in blood sugar levels.” It is thus likely that the combination of simvastatin and extended-release niacin in the New England Journal study caused the increased incidence of diabetic changes.
Timed-release niacin also tends to be more hepatotoxic than immediate-release niacin, causing significant increases in liver enzymes and multiple reports of hepatic failure. (19,20) One report, which illustrated the comparative safety of immediate-release niacin involved three patients who incurred hepatitis from timed-release niacin, who were later re-challenged with immediate-release niacin with no evidence of hepato-cellular injury due to the immediate release niacin. (21)
Statins are known to cause myalgias, fatigue and rhabdomyolysis. These effects may be worsened by combining statins with niacin. Most of the excess musculoskeletal adverse events in the New England Journal report were due to myopathy and the absolute excess of myopathy associated with adding niacin-laropiprant to the statin-ezetimibe therapy was more than 10 times as great among participants in China as those in Europe. (1) This should not have been surprising. The Zocor/Simvastatin package insert warns: “Cases of myopathy/rhabdomyolysis have been observed with simvastatin co-administered with lipid-modifying doses (more than 1 g/day) of niacin-containing products. In particular, caution should be used when treating Chinese patients with simvastatin doses exceeding 20 mg/day co-administered with lipid-modifying doses of niacin-containing products.”
The New England Journal study concluded that “treatment with extended-release niacin-laropiprant did not significantly reduce the risk of major vascular events but did significantly increase the risk of serious adverse events.” (1)
The highly-publicized New England Journal article was thus not a true study of the clinical efficacy of over-the-counter immediate-release niacin. It was, instead, a testament that it’s probably not a good idea to combine extended-release niacin with a pharmaceutical hodge-podge of a high potency statins, ezetimibe and latanoprost.
I’d like to see a head-to-head 3-arm study comparing the efficacy and side-effects of (1) immediate release niacin, (2) a statin and (3) a statin plus niacin. Until such a study is conducted, I will continue to use (and recommend to my patients) immediate-release niacin—which I believe to be the safest, cheapest, most effective lipid-lowering substance available.
Ward Dean, M.D.
References
1. Landray, MJ, Haynes, R, Hopewell, J., et al. Effect of Extended-Release Niacin with Laropiprant in High-Risk Patients. NEJM, 2014, 371;3, 203-212.
2. Anderson, TJ, Boden, WE, Desvigne-Nickens, P, et al. Safety Profile of Extended-Release Niacin in the AIM HIGH Trial. NEJM, 2014, 371;3, 288-290.
3. Lloyd-Jones, DM. Niacin and HDL Cholesterol—Time to Face Facts. NEJM, 2014, 371;3, 271-273.
4. Altschul, R, Hoffer, A, Stephen, JD. Influence of nicotinic acid on serum cholesterol in man. Arch Biochem biophys 1955; 54:558-9.
5. Canner, PL, Berge, KG, Wenger, NK, et al. Fifteen year mortality in Coronary Drug Project patients: Long term benefit with niacin. J Am Coll Cardiology 1986;8:1245-1255.
6. Miller, M. Niacin as a component of combination therapy for dyslipidemia. Mayo Clin Proceedings 2003;78:735-742.
7. Illingworth, DR, Stein, EA, Mitchel, YB, et al. Comparative effects of Lovastatin and Niacin in primary hypercholesterolemia. Arch Intern Med 1994; 154:1586-1595.
8. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High lood Cholesterol in Adults. Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults: Final report. Circulation 2002;106:3143-3421.
9. Knopp, RH. Drug treatment of lipid disorders. NEJM 1999;341:498-511.
10. The AIM-HIGH Investigators. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. NEJM 2011; 365:2255-67.
11. Lai, E, Schwartz, JI, Dallob, A, et al. Effects of extended release niacin/laropiprant, laropiprant, extended release niacin and placebo on platelet aggregation and bleeding time in healthy subjects. Platelets 2010; 21:191-8.
12. Dallob, A, Luo, WL, Luk, JM, et al. The effects of laropiprant, a selective prostaglandin D2 receptor antagonist, on the antiplatelet activity of clopidogrel or aspirin. Platelets 2011;22:495-503.
13. Food and Drug Administration. FDA drug safety communication: important safety label changes to cholesterol-lowering statin drugs. 2012. www.fda.gov/drugs/drugsafety/ucm293101.htm
14. Sattar. M, Preiss, D, Murray, HM, et al. Statins and risk of diabetes; a collaborative meta-analysis of randomized statin trials. Lancet 2010;375:735-42.
15. Preiss, D, Seshasai, SR, Welsh, P, et al. Risk of diabetes with intensive-dose compared with moderate-dose statin therapy. JAMA 2011;305:2556-64.
16. Dormuth, CR, Filion, KB, Peterson, JM, et al. Higher potency statins and the risk of new diabetes: Multicenter, observational study of administrative databases. BMJ 2014; 348:g3244.
17. Elam, MB, Hunninghake, DB, Davis, KB, et al. Effect of niacin on lipid and lipoprotein levels and glycemic control in patients with diabetes and peripheral arterial disease. The ADMIT Study: A randomized trial. JAMA 2000;284:1263-1270.
18. Grundy, SM, Vega, GL, McGovern, ME, et al. Efficacy, safety, and tolerability of once-daily niacin for the treatment of dyslipidemia associated with type 2 diabetes. Arch Int Med 2002; 162:1568-1576.
19. McKenney, JM, Proctor, JD, Harris, S. A comparison of the efficacy and toxic effects of sustained- vs immediate-release niacin in hypercholesterolemic patients. JAMA 1994;271:672-677.
20. Mullin, GE, Greenson, JK, and Mitchell, NC. Fulminant hepatic failure after ingestion of sustained-release nicotinic acid. Ann Intern Med 1989;76:239-241.
21. Henkin, Y, Johnson, KIC, and Segrest, JP. Rechallenge with crystalline niacin after drug-induced hepatitis from sustained-release niacin. JAMA 1990; 264; 241-243.
22. NIASPAN package insert, Revised: 04/2014
I am 46 years of age. In 2009, I developed diabetes insipidus. I had an inflammation on my pituitary gland and as a result I started drinking lots of very cold water with ice. I gained over 20 kg in a few months. I am continuing to experience weight gain, can’t control my weight and I still wake up in the night and drink lots of water, ½ liter at a time. I feel depressed and I don’t sweat. My endocrinologist gave me thyroxin for my thyroid. I feel better, but I’m not 100% as I once was. What supplements would you recommend for me? Looking forward to hearing from you.
I.C., Australia
Dear Mrs. I.C.,
Diabetes insipidus is indeed due to pituitary dysfunction, specifically to a loss of anti-diuretic hormone produced by the posterior pituitary for whatever reason. Often, it can result following delivery of a baby. For those not familiar with the condition, diabetes insipidus is similar to someone who urinates excessively after drinking alcohol, (because alcohol inhibits the production of anti-diuretic hormone). Of course, with alcohol use, the condition is self-limited by discontinuing alcohol ingestion. Unfortunately, in your case, the pituitary isn’t doing its job, for some reason.
Therapeutically, I suggest you add vasopressin (or desmopressin) to your daily regimen, once or twice per day, as needed. For convenience, I suggest especially at bedtime, to help you sleep without bathroom interruptions.
Second, I’m sure your endocrinologist is adjusting your dose of thyroid based on your blood tests, rather than how you are really doing. I believe that thyroid blood tests are usually a waste of blood—and that the dose of thyroid replacement should be based on how the patient is doing, and whether the thyroid-related spectrum of symptoms are resolving, while monitoring the heart rate and body temperature, as described by Dr. Rick Wilkinson, in his article, The Epidemic of Low Thyroid Diseases, in Aging Matters™ Magazine, issue # 4, 2014.1
I generally use Armour® or one of the other natural forms of thyroid, instead of thyroxine (T4, the inactive form of thyroid hormone, must be de-iodinated to T3 to become active). Titrate the dose upwards, progressively over weeks to months, until you arrive at a dose with which you are comfortable, and relatively symptom-free, with a normal (65-75 beats/minute) heart rate and normal temperature. If your thyroid hormone level is inadequate, you will have an extremely difficult time trying to normalize your weight. Also, depression is a hallmark of hypothyroidism and is one of the first symptoms to be relieved with appropriate doses of thyroid.
I also suggest metformin, 500 mg three times per day. If you have read much of my material, based on the works of Prof. Vladimir Dilman, you will know that metformin is a “metabolic rejuvenator,” that restores hypothalamic (and pituitary) receptor sensitivity to insulin, cortisol, and other hormones. Metformin is an integral component of the weight loss program that I implement in my clinic. Metformin normalizes insulin and enhances its effectiveness, generally resulting in significant weight loss in my overweight patients.
Another component that I often recommend is acarbose. Acarbose is an alpha-glucosidase inhibitor—in layman’s language, it is a starch blocker—i.e., it blocks the conversion of complex carbohydrates into glucose and delays their absorption, resulting in overall reduced glucose spikes, and reduced caloric absorption. When used with metformin, acarbose greatly enhances weight loss. I recommend 100 mg three times per day, with meals (or carbohydrate-laden snacks), make sure you chew the tablets not swallow them.
I believe that with the combination of vasopressin (to assist your pituitary), increasing your dose of thyroid, and adding Metformin and Acarbose to your regimen will greatly alleviate your thirst and excessive diuresis, weight gain and depression.
In addition, I have been reliably informed that the Russian peptide bioregulator for the bladder, called Chitomur® is a useful adjunct to reduce urination. I don’t have personal experience of this yet, but considering the safety profile of these peptides could well be worth a try.
Let me know how you do,
Ward Dean, M.D.
[Editor- IAS provides acarbose as 100 mg tablets branded Glucobay®, metformin is available from IAS as Metforal® 500 mg tablets and also in SR (slow release) tablets; vasopressin is available in nasal spray as Vaso-Pro™ and desmopressin is available as a nasal spray as Minurin®].
1. Wilkinson, R. The Epidemic of Low Thyroid Diseases, Aging Matters Magazine, No5, 2014 # 4-9.
2. Standl, E, and Schnell, O. Alpha-glucosidase inhibitors 2012- Cardiovascular considerations and trial evaluation. Diabetes & Vascular Diseases Research, 2012; 9:(3) 163-169.
My 18-year old son has been diagnosed with ADHD, he has not been prescribed anything yet- but I have heard bad things about amphetamine drugs like Ritalin®. I would greatly appreciate your advice on better medicines and nutrition that could help him instead? Thank you very much.
A.S., Arizona
Dear Mrs. A.S.,
Stimulants like Ritalin® are effective in controlling the symptoms of Attention-Deficit/Hyperactivity Disorder (ADHD). Unfortunately, they are, of course, addictive Schedule II controlled substances, with side effects of their own—and are ineffective in about 30% of users. Fortunately, there are a number of other medications and natural substances that address the cause of his condition and may enable your son to avoid psycho-stimulants like Ritalin and Adderall®.
DMAE or centrophenoxine
For children (and adults) who suffer from ADHD (and even for those who don’t), I recommend DMAE (dimethylaminoethanol). DMAE has been used for over half a century to improve behavioral disorders in children, and may have positive effects on intelligence and grades as well. In 1958, Dr. Leon Oettinger, Jr., reported that DMAE:
- Accelerated mental processes
- Improved concentration span
- Abolished early morning fogginess
- Relieved lassitude and mild depression with obvious letdown when it was discontinued
- Was useful in schizophrenia of long duration (with prolonged treatment)
- Decreased irritability and reduced over-activity, leading to a much better overall social adaptation and improved scholastic functioning
- Increased attention span
- Did not cause drowsiness
- Improved IQ!
Furthermore, he found that DMAE had numerous advantages over the amphetamines (like Ritalin) in that there were no effects on heart rate or blood pressure, and no induced jitteriness. Instead of causing anorexia (loss of appetite) like the amphetamines, he found that DMAE actually improved appetite in many patients and caused no interference with sleep. In fact, he reported that DMAE actually reduced sleep requirements. Dr. Oettinger concluded that; “DMAE was a most useful tool in the handling of children with behavioral problems.” (1) In 1960, Dr. Stanley Geller conducted a double-blind study of seventy-five children. DMAE in doses of 50 mg twice daily resulted in improved functioning capacity, puzzle-solving ability and organizational activity. (2) Another double-blind study compared DMAE with both methylphenidate (Ritalin®) and placebo in seventy-four children with unspecified “learning disabilities” (what we would probably call ADHD today). The study found significant test score improvement for both treatment groups over a 10-week period. (3) In another double-blind study of fifty children with “hyperkinetic syndrome,” DMAE was administered in doses up to 500 mg/day. The author concluded that DMAE, at doses of 300-500 mg per day for 12 weeks to moderately disturbed hyperkinetic children produced greater overall improvement compared to patients treated with a placebo. (4) Although human studies were rare after the late 70s, due to DMAE’s loss of patent protection, more recent studies have confirmed its benefits and mechanisms. A 1995 study from Duke University found that rats given DMAE showed improvements in their working memory performance, (5) and a more recent study from 2003 involved eighty students with “borderline emotional disturbance.” The subjects were given either a placebo or a vitamin/mineral mixture which contained DMAE bitartrate. The subjects taking the vitamin/mineral/DMAE mixture had a greater increase in well-being and improvement in mood and attention compared to those taking the placebo. (6)
Centrophenoxine (Lucidril®, Centro-Pro™, meclofenoxane) was developed in 1959, and has been called a “brain metabolic stimulant” and a neuroenergizer). (7) Scientists from India declared it to be a neurorejuvenator. (8) Centrophenoxine stimulates glucose uptake, oxygen consumption, and cerebral electrical activity in the brain. Increased brain metabolic and electrical activities are the basis for improved attention and alertness. Clinical studies with centrophenoxine in patients with confusion and disturbances of memory and concentration markedly improved after several weeks of treatment. Studies in Europe reported significant improvement of fatigue, irritability, confusion and memory dysfunction with centrophenoxine. (9) Centrophenoxine is a combination of DMAE and PCPA (paarachlorophenoxyacetic acid). Pharmacokinetic studies revealed that much higher levels of DMAE were found in the brain after centrophenoxine treatment compared to DMAE alone, since the DMAE with PCPA penetrates the blood-brain barrier much easier. (10) Centrophenoxine is, in effect, a super-DMAE. Thus, centrophenoxine can be expected to provide even better results in improving attention. Centrophenoxine doses are typically 250–1,000 mg twice daily (breakfast and lunch). For use in enhancing focus and attention span, where no major brain pathology is present, 250 mg once or twice daily is a generally safe and useful dose.
The alerting drug modafinil shares many apparent similarities with amphetamines, (although with fewer adverse side effects and less potential for addiction or abuse). Also, because of modafinil’s effects on cognition, its efficacy in treating ADHD has been extensively studied. One of the first studies for ADHD compared modafinil (200 mg/day) with amphetamine and placebo in twenty-two adults. Modafinil and amphetamines were both found to improve ADHD behavior.(11) In a continuing series of studies, modafinil improved ADHD symptoms in eleven children on average doses of 200 mg/day (range 100–400 mg);(12) twenty-two children with ADHD, taking modafinil in doses ranging from 200–300 mg /day, exhibited greater improvement than the placebo group;(13) twenty adults with ADHD on modafinil 200 mg showed enhanced performance on a number of standard psychological tests; (14) 164 children and adolescents with ADHD, taking 270 mg of modafinil/day (range 170–425 mg), showed greater improvements than the placebo-treated group. (The differences in symptoms were apparent from the first week of treatment and were maintained throughout the study);(15) another large study of childhood ADHD (100 in the modafinil-treated group and 41 in the placebo group), with an average dose of 360 mg modafinil, again demonstrated reduced ADHD symptoms at school and home;(16) 223 children (aged 6–13 years) receiving modafinil showed a greater improvement in all three of the major ADHD rating scales; (17) and 190 ADHD patients (aged 6–17 years) showed greater improvement in the modafinil-treated groups (receiving either 340 mg or 425 mg, based on body weight) than placebo (18). In a summary review of modafinil use in ADHD, scientists from the Department of Psychiatry, University of California, San Diego, reviewed 33 double-blind placebo controlled trials of modafinil, in addition to numerous smaller studies and case reports. They concluded that “Modafinil is a promising drug with a large potential for many uses in psychiatry and general medicine,” and that “the strongest evidence among off-label uses exists for the use of Modafinil in attention-deficit disorder.”(19)
Note: An earlier version of modafinil is adrafinil (Adra-Pro™) it isn’t quite as effective as modafinil and can have more side effects; however it is still very effective and considerably cheaper than modafinil. A typical adrafinil dose could be 300 mg once or twice daily, although it is not recommended to use continuously for 3-months without monitoring liver enzyme levels.
Vitamins B6, D, and magnesium
Nutritional supplements may also be of help—especially magnesium, and Vitamins D and B6. Fifty hyperactive children (ages 7-12) were all found to be deficient in magnesium (determined by serum and intracellular erythrocyte levels; and hair analysis with atomic absorption spectroscopy). 30 were treated with 200 mg magnesium/day for six months. Twenty were treated with a placebo. Those treated with magnesium experienced normalization of magnesium and decreased hyperactivity, compared to their previous clinical state and to the control group. (20) In a more recent study, 36 children with ADHD who were also low in erythrocyte magnesium levels compared to normal (control) children were treated with 200 mg magnesium and 20 mg vitamin B6 each day for 8 weeks. The authors reported a significant increase in erythrocyte magnesium levels, and significantly improved behavioral and school attention symptoms. (21) Two very recent studies examined Vitamin D levels in students with ADHD, and found those with ADHD to have dramatically lower blood levels than the normal students. (22, 23)
Herbs for ADHD; Ginkgo biloba, ginseng and pycnogenol
Because ginkgo biloba has been traditionally used in the treatment of dementia and memory impairment, scientists hypothesized that it might be beneficial for those with ADHD. In a double blind comparison of ginkgo and methylphenidate (Ritalin®), fifty students with ADHD (39 boys and 11 girls) were treated with 80-120 mg/day gingko or 20-30 mg/day methylphenidate, (based on subjects’ weight) for a 6 week double blind trial. Although ginkgo was more effective than placebo, it was less effective than methylphenidate in the treatment of ADHD. (24) A year later, an Italian scientist administered ginkgo to six patients with ADD. The author noted significant improvement in hyperactivity, inattention, and immaturity factors and concluded that ginkgo might be a beneficial and useful treatment of ADD, with minimal side effects. (25) In Korea, scientists investigated the effects of Korean red ginseng on ADHD. Eighteen students were administered 1,000 mg of ginseng twice daily for eight weeks. At the conclusion of the study, significant improvements were noted in all rating scales. The authors concluded that; “Korean red ginseng may be effective in improving inattentiveness in those with ADHD.”(26) In 2001, Canadian scientists presciently studied the effects of a combination of ginkgo biloba extract and American ginseng on ADHD. Curiously, they used only 200 mg of American ginseng and 50 mg of ginkgo biloba extract twice daily. Despite these pathetically low doses, they found dramatic improvements in the three ADHD rating scales used. The authors concluded that the ginkgo-ginseng combination may improve symptoms of ADHD. (27) I believe the results would have been even more dramatic if optimum dosages (1,000 mg of ginseng, and 120 mg of ginkgo, each twice daily) had been used. Pycnogenol® is the trade name for French maritime pine bark extract; Pycnogenol acts as a vasodilator, which improves cerebral blood flow to brain regions involved in ADHD, (28) and regulates catecholamine levels among ADHD children. (29)
In a study to evaluate the effect of Pycnogenol on ADHD symptoms, sixty-one children with ADHD were supplemented with 1 mg/kg/day Pycnogenol or placebo over a period of 4 weeks. Pycnogenol administration caused a significant reduction of hyperactivity, improved attention, and improvement of fine motor coordination and concentration of children. (29) Lead, cell phones, and chelation Lead intoxication has been strongly associated with ADHD. Blood lead above 10 μg/dL had been reliably associated with ADHD and related behaviors–the only real dispute was to determine if there was a safe level of lead. (30-32) Subsequent studies indicated that even very low levels of blood lead (2-10 μg/dL) are associated with ADHD. (33-35) In 2013, a team of Korean scientists conducted a large, (nearly 2,500 students) 2 year-long study and found that simultaneous exposure to lead and RF from mobile phone use was associated with increased ADHD symptom risk.(36) I recommend that those with ADHD minimize the use of cellphones and undergo oral and/or IV chelation therapy with EDTA.
[Ed.- EDTA is available in BCI®, EDD® and also in Beyond Clean2® bath salts].
Conclusion:
To sum everything up, I recommend appropriate doses of DMAE or Centrophenoxine; if your budget allows, modafinil 100 mg in the morning, and another 100 mg in early afternoon; (alternatively the adrafinil), magnesium 200-400 mg per day (or to bowel tolerance—excessive magnesium will cause GI upset or diarrhea); Vitamin D3 5,000 IU/day; Vitamin B6 200 mg/day; Ginseng 1,000 mg twice daily; Ginkgo biloba 120 mg twice daily and Pycnogenol 50-100 mg/day. I suggest starting with one supplement at a time, adjust the dose to your son’s response/tolerance and then introduce other supplements sequentially (If he starts with everything all at once, it will be difficult to identify what is working, or what is causing an adverse side effect, (although side effects with any of these substances are neither serious nor common).
Finally, because of the adverse effects of any amount of lead, I again recommend oral and/or IV chelation therapy with EDTA and based on the conclusive results from the Korean scientists, I recommend minimal use of cellphones, and use of various shielding devices to minimize microwave exposure such as RF-blocking protective cases and air-tube headsets.
Ward Dean, M.D.
References
1. Oettinger, L. The use of Deanol in the treatment of disorders of behavior in children. J. Pediat, 1958, 53: 761-675.
2. Geller, S. J. Comparison of a tranquilizer and a psychic energizer. JAMA, 1960, 174: 89-92.
3. Lewis JA, Young R. Deanol and methylphenidate in minimal brain dysfunction. Clin Pharmacol Ther. 1975 May;17(5):534-40.
4. Coleman, N., Dexheimer, P., Dimascio, A., Redman, W., and Finnerty, R. Deanol in the treatment of hyperkinetic children. Psychosomatics, 1976, 17: 68-72.
5. Levin ED, Rose JE, Abood L. Effects of nicotinic dimethylaminoethyl esters on working memory performance of rats in the radial-arm maze. Pharmacol Biochem Behav. 1995 Jun-Jul;51(2-3):369-73.
6. Dimpfel W, Wedekind W, Keplinger I. Efficacy of dimethylaminoethanol (DMAE) containing vitamin-mineral drug combination on EEG patterns in the presence of different emotional states. Eur J Med Res. 2003 May 30;8(5):183-91.
7. South, J. “Lucidril- The Anti-Aging Neuro-Energizer.” IAS Anti-Aging Bulletin. 2001 4(9), 31-39.
8. Sharma D, Maurya, AK, and Singh, R. Age-related decline in multiple unit action potentials of CA3 Region of Rat hippocampus: Correlation with lipid peroxidation and liposfuscin concentration and the effect of centrophenoxine. Neurobiology of Aging, 1993, 14:319-330.
9. Zs.-Nagy, I. “A Survey of the Available Data on a New Nootropic Drug, BCE-001″ Ann NY Acad Sci. 1994. 717, 102-14.
10. Nandy, K. (1978) “Centrophenoxine: Effects on Aging Mammalian Brain” J Am Ger Soc 26, 74-81.
11. Taylor FB, Russo J. Efficacy of modafinil compared to dextroamphetamine for the treatment of attention deficit hyperactivity disorder in adults. J Child Adolesc Psychopharmacol. 2000 Winter;10(4):311-20.
12. Rugino TA, Copley TC. Effects of modafinil in children with attention-deficit/hyperactivity disorder: an open-label study. J Am Acad Child Adolesc Psychiatry. 2001;40 :230– 235
13. CrossRefMedlineWeb of Science
14. Rugino TA, Samsock TC. Modafinil in children with attention-deficit hyperactivity disorder. Pediatr Neurol. 2003; 29 :136– 142 CrossRefMedlineWeb of Science
15. Turner DC, Clark L, Dowson J, Robbins TW, Sahakian BJ. Modafinil improves cognition and response inhibition in adult attention-deficit/hyperactivity disorder. Biol Psychiatry 2004; 55: 1031–1040.
16. Biederman J, Swanson JM, Wigal SB, et al. Efficacy and safety of modafinil film-coated tablets in children and adolescents with attention-deficit/hyperactivity disorder: results of a randomized, double-blind, placebo-controlled, flexible-dose study. Pediatrics. 2005; Dec;116(6):e777-84.
17. Greenhill LL, Biederman J, Boellner SW, Rugino TA, Sangal RB, Earl CQ et al (2006). A randomized, double-blind, placebo-controlled study of modafinil film-coated tablets in children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 45: 503–511.
18. Biederman J, Swanson JM, Wigal SB, Boellner SW, Earl CQ, Lopez FA (2006). A comparison of once-daily and divided doses of modafinil in children with attention-deficit/hyperactivity disorder: a randomized, double-blind, and placebo-controlled study. J Clin Psychiatry 67: 727–735.
19. Swanson JM, Greenhill LL, Lopez FA, Sedillo A, Earl CQ, Jiang JG et al. Modafinil film-coated tablets in children and adolescents with attention-deficit/hyperactivity disorder: results of a randomized, double-blind, placebo-controlled, fixed-dose study followed by abrupt discontinuation. J Clin Psychiatry 2006;67: 137–147.
20. Ballon JS, Feifel D. A systematic review of modafinil: Potential clinical uses and mechanisms of action. J Clin Psychiatry. 2006;67(4):554-66.
21. Starobrat-Hermelin B, Kozielec T. The effects of magnesium physiological supplementation on hyperactivity in children with attention deficit hyperactivity disorder (ADHD). Positive response to magnesium oral loading test. Magnes Res. 1997 Jun;10(2):149-56.
22. Mousain-Bosc M, Roche M, Polge A, et al. Improvement of neurobehavioral disorders in children supplemented with magnesium-vitamin B6. I. Attention deficit hyperactivity disorders. Magnes Res. 2006 Mar;19(1):46-52.
23. Kamal M, Bener A, Ehlayel MS. Is high prevalence of vitamin D deficiency a correlate for attention deficit hyperactivity disorder? Atten Defic Hyperact Disord. 2014 Jun;6(2):73-8. doi: 10.1007/s12402-014-0130-5. Epub 2014 Mar 9.
24. Goksugur SB, Tufan AE, Semiz M, et al. Vitamin D status in children with attention-deficit-hyperactivity disorder. Pediatr Int. 2014 Aug;56(4):515-9. doi: 10.1111/ped.12286. Epub 2014 Jun 17.
25. Salehi B, Imani R, Mohammadi MR, et al. Ginkgo biloba for attention-deficit/hyperactivity disorder in children and adolescents: a double blind, randomized controlled trial. Prog Neuropsychopharmacol Biol Psychiatry. 2010 Feb 1;34(1):76-80. doi: 10.1016/j.pnpbp.2009.09.026. Epub 2009 Oct 5.
26. Niederhofer H. Ginkgo biloba treating patients with attention-deficit disorder. Phytother Res. 2010 Jan;24(1):26-7. doi: 10.1002/ptr.2854.
27. Lee SH, Park WS, and Lim MH. Clinical Effects of Korean Red Ginseng on Attention Deficit Hyperactivity Disorder in Children: An Observational Study. J Ginseng Res. Jun 2011; 35(2): 226–234. doi: 10.5142/jgr.2011.35.2.226
28. Lyon MR, Cline JC, Totosy de Zepetnek J, et al. Effect of the herbal extract combination Panax quinquefolium and Ginkgo biloba on attention-deficit hyperactivity disorder: a pilot study. J Psychiatry Neurosci. May 2001; 26(3): 221–228.
29. Rucklidge JJ, Johnstone J, Kaplan BJ. Nutrient supplementation approaches in the treatment of ADHD. Expert Review of Neurotherapeutics. 2009;9(4):461–476.
30. Trebatická J, Kopasová S, Hradecná Z, et al. Treatment of ADHD with French maritime pine bark extract, Pycnogenol. Eur Child Adolesc Psychiatry. 2006 Sep;15(6):329-35. Epub 2006 May 13.
31. Silva PA, Hughes P, Williams S, Faed JM. Blood lead, intelligence, reading attainment, and behaviour in eleven year old children in Dunedin, New Zealand. Journal of Child Psychology and Psychiatry. 1988;29:43–52.
32. Thomson GO, Raab GM, Hepburn WS, Hunter R, Fulton M, Laxen DP. Blood-lead levels and children’s behavior results from the Edinburg Lead Study. Journal of Child Psychology and Psychiatry. 1989;30:515–528.
33. Burns JM, Baghurst PA, Sawyer MG, McMichael AJ, Tong S. Lifetime low-level exposure to environmental lead and children’s emotional and behavioral development at 11–13 years: The Port Pirie Cohort Study. American Journal of Epidemiology. 1999;149:740–749.
34. Braun J, Kahn RS, Froehlich T, Auinger P, Lanphear BP. Exposures to environmental toxicants and attention deficit hyperactivity disorder in U.S. children. Environmental Health Perspective. 2006;114:1904–1909.
35. Nigg JT, Knottnerus GM, Martel MM, Nikolas M, Cavanagh K, Karmaus W, Rappley MD. Low blood lead levels associated with clinically diagnosed attention-deficit/hyperactivity disorder and mediated by weak cognitive control. Biological Psychiatry. 2008;63:325–331.
36. Nigg, JT, Nikolas MA, Knottnerus,GM, et al. Confirmation and Extension of Association of Blood Lead with Attention-Deficit/Hyperactivity Disorder (ADHD) and ADHD Symptom Domains at Population-Typical Exposure Levels. J Child Psychol Psychiatry. Jan 2010; 51(1): 58–65. doi: 10.1111/j.1469-7610.2009.02135.x
37. Byun YH, Ha M, Kwon HJ, et al. Mobile phone use, blood lead levels, and attention deficit hyperactivity symptoms in children: a longitudinal study. PLoS One. 2013;8(3):e59742. doi: 10.1371/journal.pone.0059742. Epub 2013 Mar 21.
Dear Dr. Dean,
I started taking one grain (60 mg) Armour thyroid per day on November 25, 2014. On December 18 (about 3 ½ weeks later), I increased the dose to two grains per day. I know that it takes a while to work. In the meantime, I am experiencing bloody diarrhea. I presume that this is a side effect of my abnormal thyroid.
I would like to know if you have anything to stop or slow these symptoms down until my thyroid gets back to normal. I would welcome any advice.
Thank you so much,
Louise
Dear Louise,
Rectal bleeding is not associated with thyroid dysfunction, nor with thyroid replacement therapy. I think you’ve got something else going on. I strongly recommend that you see a physician to determine the cause of your bloody diarrhea.
While you are adjusting your dose of Armour thyroid, I recommend that you monitor your basal temperature and heart rate—placing special emphasis on your resting heart rate. “Normal” heart rate is about 72 beats per minute—and somewhat less in well-conditioned athletes (marathon runners may have a resting heart rate in the 40s or low 50s). If your heart rate spikes into the 80s or 90s, I suggest reducing your dose of thyroid.
Please let me know what you find out.
Sincerely,
Ward Dean, MD
Do you have the symptoms of hypothyroidism?
1. Sensitivity to cold – especially in the hands and feet 2. Fatigue – reduced energy levels 3. Weight gain 4. Inability to lose weight despite constant dieting 5. Infections – especially respiratory infections 6. Frequent bouts of cold or flu 7. Asthma and allergies 8. Decreased perspiration 9. Dry, coarse, leathery skin; pale 10. Poor circulation 11. Coarse hair or hair loss 12. Dry eyes – blurred vision 13. Swelling or puffy eyelids 14. Digestive problems, irritable bowel syndrome, or acid indigestion 15. Constipation 16. Headaches – moderate to severe 17. Poor short term memory and concentration 18. Arthritis, joint pains 19. Low blood pressure 20. High blood pressure 21. High cholesterol or atherosclerosis 22. Diabetes 23. Hypoglycemia 24. Low libido 25. Anxiety – panic attacks 26. Depression – moderate to severe 27. Behavioral and emotional disorders 28. Wounds that heal slowly 29. Menstrual problems (include PMS or hysterectomy) 30. Infertility 31. Enlarged thyroid-goiter 32. Acne 33. Lateral halves of eyebrows missing
Figure 1: Hypothyroidism is a condition of insufficient output from the thyroid gland. Broda Barnes, M.D., Ph.D., (perhaps the most famous thyroid researcher and author of Hypothyroidism: The Unsuspected Illness), reports that the symptoms related to low thyroid vary widely and may include those shown in the table. Why not check all that apply to you?
References
Barnes B, and Galton, L. Hypothyroidism, the Unsuspected Illness. 1972, Harper and Row, New York 2. Goldberg JB, Kurland AA. Dilantin treatment of hospitalized cultural-familial retardates. J Nerv Ment Dis. 1970 Feb;150(2):133-7. 3. Daniel R. Psychiatric drug use and abuse in the aged. Geriatrics. 1970 Jan;25(1):144-5. 4. Smith WL, Lowrey JB. Effects of diphenylhydantoin on mental abilities in the elderly. J Am Geriatr Soc. 1975 May;23(5):207-11. 5. Kim D. Practical Use and Risk of Modafinil, a Novel Waking Drug. Environ Health Toxicol. 2012; 27.
Dear Dr. Dean,
May I please have your opinion on the relevance of piracetam as a smart drug? Do you feel that it still ‘stands up’ despite being many decades old, and have any of the new nootropics surpassed it in anyway?
S.F., California
Dear SF.
That’s a very good question. As you said, piracetam has been around for a long time – since 1972. I first learned about piracetam in Korea, (where I graduated from medical school in 1978). At that time, carbon monoxide poisoning was a common occurrence, due to leakages from the Korean in-floor heating systems. The standard method of treatment was a combination of intravenous piracetam and hyperbaric oxygenation. Although piracetam has been available generically for many years, research into its properties for a wide range of clinical conditions has continued. In Hungary in 2000, a Phase IV clinical study of 104 patients with mild cognitive impairment-dementia participated in a double-blind study of piracetam, 4800 mg/day for 4 weeks, followed by 2400 mg/day thereafter. Five factors of the modified Mini-Mental State examination were evaluated. Nearly all factors significantly improved with piracetam- especially memory, concentration and psychomotor speed. The cognitive enhancement effects appeared in a few weeks, and were most pronounced in patients with depressive symptoms. (1) Belgian scientists in 2002 conducted a meta-analysis of nineteen double-blind studies of patients suffering from dementia or age-related cognitive impairment treated with piracetam. The authors concluded that the treatment demonstrated meaningful clinical improvement, with compelling evidence for the global efficacy of piracetam. (2)
In 2005, Polish scientists reviewed the documented benefits of piracetam, affirming that it improves alertness, learning, memory, brain metabolism and capacity. They reported that piracetam alters plasma membrane properties by increasing membrane fluidity and protects the cell against hypoxia, increases red cell deformability and normalizes hyperactive platelet aggregation, resulting in anti-thrombotic, neuroprotective and rheological properties. The scientists theorized that these properties resulted in the efficacy of piracetam in various disorders including dementia, vertigo, sickle cell anemia, myoclonus and stroke, improves reading comprehension and accuracy in dyslexic children, socialization and IQ in elderly psychiatric patients, and is even used to treat alcoholism. (3)
Also in 2005, piracetam’s properties were reviewed by a scientist from the Karolinska Institute in Sweden, who echoed the above review from Poland. (4)
In 2014, a team of Chinese scientists conducted a meta-analysis of three studies of piracetam used preventively prior to coronary artery bypass grafting (CABG). (5) Cognitive dysfunction of varying degrees is an unfortunately too-common side effect of this procedure. Between 25 and 80% of patients who undergo CABG surgery develop postoperative cognitive dysfunction (POCD), ranging from slight to pronounced disturbances that may persist for several weeks up to several years. Three studies were identified- two in Germany and one in Romania – in which piracetam was administered prior to surgery to prevent the resultant cognitive dysfunction.
In the first trial in 2003 in Germany, physicians administered 12 gm piracetam (or saline, placebo) via IV infusion to 64 patients 3 hours prior to undergoing bypass surgery. The authors reported that the piracetam-treated patients produced a better level of performance in short-term memory and attention 3-days after surgery, compared to the placebo group. (6)
In 2006, Romanian physicians administered piracetam or placebo intravenously (150 mg/kg daily; 300 mg/kg on the day of surgery) to 98 patients, from the day before surgery to 6-days after surgery, then orally (12 g/day) up to 6 weeks after surgery. The authors reported that six weeks after CABG, cognition was significantly improved in those treated with piracetam compared to placebo. (7) In 2008, another team of German physicians performed a third study of piracetam’s ability to prevent cognitive dysfunction due to bypass surgery. This study was the largest, comprised of 120 patients, each of whom received 12 grams of piracetam or placebo just prior to the surgery. Again, the piracetam patients performed significantly better compared to the placebo patients after the operation, and had less decline of overall cognitive function. (8)
From 2010-2013, a series of papers was produced by an international team including scientists from Germany, Italy, France, Switzerland, China, Australia and the U.S., who investigated the mitochondrial resuscitating mechanisms of piracetam as a further explanation of its neuroprotective properties. In the first paper in this series, the authors showed that piracetam prevented decreases in mitochondrial membrane potential (MMP) and fall in ATP production associated with β-amyloid accumulation, suggesting that improving mitochondrial function protected against the neurodegeneration induced by β-amyloid (Aβ) (involved in Alzheimer’s disease). The brains of animals treated with piracetam showed markedly decreased loads of Aβ. Aβ-induced mitochondrial dysfunction also causes impairment of neuritogenesis and the Aβ-induced reduction of neurite growth was substantially improved by piracetam. The authors concluded that piracetam’s ability to improve mitochondrial function was a valid approach to ameliorate the detrimental effects of Aβ on brain function. (9)
In the second paper, the authors reviewed piracetam’s ability to improve interhemispheric transfer, enhance cerebral resistance to hypoxia, (as I observed in Korea during treatment of carbon monoxide poisoning) and most importantly, to facilitate learning and other cognitive functions. The authors reported that the cognition-improving properties represent the most common therapeutic use of piracetam all over the world – i.e., memory disorders, impaired cognitive functions after head injuries, and vertigo. In over four decades of piracetam’s clinical use, the cognition-improving properties have been found to be more pronounced when brain function is impaired, by aging, hypoxia, cerebral injuries, or Aß load in Alzheimer’s disease. The authors concluded that after more than 40 years’ use of piracetam, the new findings of mitochondrial protection provide a new perspective for this old nootropic and explain its continued use in many countries around the world. (10)
In a third paper, the scientists again demonstrated that piracetam improved MMP (mitochondrial membrane potential), elevated mitochondrial ATP production, enhanced neurite outgrowth and reduced Aβ levels in several cell models (in vitro) as well as in mice (in vivo). They concluded that piracetam, (which they referred to as a “metabolic enhancer”) improves mitochondrial function following mitochondrial impairment typical for brain aging and early stages of AD. (11) Piracetam has never been approved for clinical use in the U.S. Thus, it’s not surprising that all of the above-cited papers were from elsewhere. Nevertheless, in 2010, scientists from NovoMed Consulting, in Silver Spring, Maryland, aware of the increasing interest in nootropic drugs for the treatment of CNS disorders, undertook an analysis of evidence-based clinical investigations of piracetam performed during the previous ten years. They conducted a literature search of the following therapeutic categories of CNS disorders: (i) cognition/memory; (ii) epilepsy and seizure; (iii) neurodegenerative diseases; (iv) stroke/ ischemia; and (v) stress and anxiety. The scientists were unable to confirm that piracetam exhibited long-term benefits for mild cognitive impairments, but they affirmed the studies demonstrating piracetam’s neuroprotective effect during coronary bypass surgery and its efficacy in treating cognitive disorders of cerebrovascular and traumatic origin; and they found piracetam’s overall effect on lowering depression and anxiety was even higher than improving memory. As an add-on therapy, piracetam appeared to benefit individuals with myoclonus, epilepsy and tardive dyskinesia and when used in combination with a vasodilator drug, piracetam appeared to have an additive beneficial effect on various cognitive disabilities. (12) Piracetam’s sales continue to rise. The most recent data I could find (from 2010-2011), indicated world-wide sales in 2011 were in excess of $120 million, with an approximate increase in sales of about 8% from 2010 (Figure 2).
Although piracetam has been around for over 40 years, research into its mechanisms and clinical effects continues. It has a safety record equaled by few pharmaceuticals and the recent identification of its mitochondria-resuscitating properties and ability to restore cell and mitochondrial membrane fluidity help to explain many of its neuroprotective and cognitive-enhancing effects and hint at its potential, (but rarely-investigated) potential as a life-extending/antiaging agent. In this regard, a Russian article reported that a combination of piracetam with a Russian cognitive-enhancer named Cerebral resulted in an increase in the lifespan and a delay in the appearance of brain degenerative processes in Drosophila melanogaster – although the flies were unaffected by Cerebral alone – implying that the life-extending effect was due entirely to piracetam. (13)
So, yes, I think piracetam still “stands up” to the competition – especially when combined with other cognitive enhancers.
Ward Dean, MD
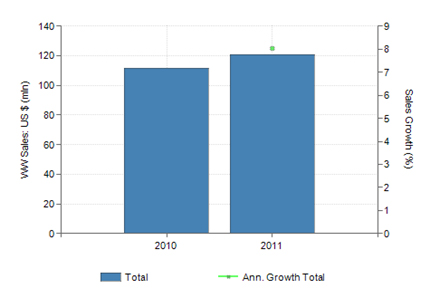
Figure 2: Global sales of piracetam are still very significant at $120 million annually and they still appear to be growing.
References
1. Tariska P, Paksy A. [Cognitive enhancement effect of piracetam in patients with mild cognitive impairment and dementia]. Orv Hetil. 2000 May 28;141(22):1189-93.
2. Waegemans T, Wilsher CR, Danniau A, Ferris SH, Kurz A, Winblad B. Clinical efficacy of piracetam in cognitive impairment: a meta-analysis. Dement Geriatr Cogn Disord. 2002;13(4):217-24.
3. Winnicka K, Tomasiak M, Bielawska A. Piracetam–an old drug with novel properties? Acta Pol Pharm. 2005 Sep-Oct;62(5):405-9.
4. Winblad B. Piracetam: a review of pharmacological properties and clinical uses. CNS Drug Rev. 2005 Summer;11(2):169-82.
5. Fang Y, Qiu Z, Hu W, et al. Effect of piracetam on the cognitive performance of patients undergoing coronary bypass surgery: A meta-analysis. Exp Ther Med. 2014 Feb;7(2):429-434. 6. Uebelhack R, Vohs K, Zytowski M, Schewe HJ, Koch C, Konertz W. Effect of piracetam on cognitive performance in patients undergoing bypass surgery. Pharmacopsychiatry. 2003 May;36(3):89-93.
7. Szalma I, Kiss A, Kardos L. Piracetam prevents cognitive decline in coronary artery bypass: a randomized trial versus placebo. Ann Thorac Surg. 2006 Oct;82(4):1430-5.
8. Holinski S, Claus B, Alaaraj N, et al. Cerebroprotective effect of piracetam in patients undergoing coronary bypass surgery. Med Sci Monit. 2008 Nov;14(11):PI53-7.
9. Kurz C, Ungerer I, Lipka U, et al. The metabolic enhancer piracetam ameliorates the impairment of mitochondrial function and neurite outgrowth induced by ß-amyloid peptide. Br J Pharmacol. May 2010; 160(2): 246–257. doi: 10.1111/j.1476-5381.2010.00656.x
10. Leuner K, Kurz C, Guidetti G, et al. Improved Mitochondrial Function in Brain Aging and Alzheimer Disease – the New Mechanism of Action of the Old Metabolic Enhancer Piracetam. Front Neurosci. 2010; 4: 44. Published online Sep 7, 2010. doi: 10.3389/fnins.2010.00044
11. Stockburger C, Kurz C, Koch KA, et al. Improvement of mitochondrial function and dynamics by the metabolic enhancer piracetam. Biochem Soc Trans. 2013 Oct;41(5):1331-4. doi: 10.1042/BST20130054.
12. Malykh AG, Sadaie MR. Piracetam and piracetam-like drugs: from basic science to novel clinical applications to CNS disorders. Drugs. 2010 Feb 12;70(3):287-312.
13. Plakhta EL, Kushnir AG, Maksimov DV, et al. [Dynamics of neurodegenerative processes and lifespan under the action of Cerebral combined with other pharmaceuticals in Drosophila melanogaster mutants]. Eksp Klin Farmakol. 2009 Mar-Apr;72(2):16-9.
Q. Dear Dr. Dean,
I am a man in my mid-50s and my job involves reading a lot of technical materials. Recently I’ve found my concentration waning and I’m easily distracted, with boredom easily upon me. Is there anything you can recommend that could help me regain my focus and concentration again?
t would be greatly appreciated.
A.M., Japan
A. Dear Mr. A.M.,
One cause of foggy thinking and poor concentration can be subclinical (or overt) hypothyroidism. See the attached list of hypothyroid symptoms in figure 1, (adapted from Dr. Broda Barnes’ book, Hypothyroidism, the Unsuspected Illness). (1) If many of the symptoms apply, you might consider treatment with Armour® thyroid, as outlined by Dr. Richard Wilkinson in his article; The Hypothyroid Epidemic, in issue #4, 2014 of the Aging Matters™ Magazine.
A second suggestion is phenytoin (Dilantin®). Although phenytoin is a time-honored anti-seizure medication, one of its lesser-known properties is its ability to restore focus and attention. A series of studies by different investigators in the 1970s demonstrated the ability of phenytoin to enhance concentration and focus. In a double-blind study of 47 “retardates,” Goldburg and Kurland reported strong improvement in ability to maintain attention and concentration, using a dose of 100 mg of phenytoin twice daily.(2) Another study, using the same dose, reported phenytoin was useful for symptoms of lack of attention and concentration.(3) A third double-blind study of the effects of 100 mg of phenytoin twice daily on the mental functions of elderly persons in the “normal-bright normal in the “middle and lower-upper socio-economic group” resulted in “significant improvement in long-term memory and social comprehension, increased ability to learn new material and increased speed in visual-motor coordination, improved general mental functioning and marked improvements in concentration.” (4)
You might also consider one of the eugorics, or “alerting drugs.” Eugeroic means good arousal. Drugs in this class include modafinil (Provigil®), armodafinil (Nuvigil®), or the less expensive prototype, adrafinil (Adra-Pro®). These drugs are psychostimulants with a waking effect, prescribed to shift workers and patients suffering from narcolepsy with cataplexy. Adrafinil was the first of this class, developed in France and still available in Europe, but which has never been approved in the U.S. Modafinil and armodafinil are analogs of adrafinil and are both available by prescription in the U.S. All of these drugs have mood-elevating and memory-enhancing effects, in addition to maintaining mental alertness. They are used “off label” to treat memory loss due to dementia, ADHD, jet lag and fatigue caused by extended work hours or illnesses. A recent article recommended that; “modafinil [and presumably the other members of this class] can be used by anyone who wishes to work late and/or concentrate for a long time.” (5)
I hope this helps,
Ward Dean, MD
Do you have the symptoms of hypothyroidism?
- Sensitivity to cold – especially in the hands and feet
- Fatigue – reduced energy levels
- Weight gain
- Inability to lose weight despite constant dieting
- Infections – especially respiratory infections
- Frequent bouts of cold or flu
- Asthma and allergies
- Decreased perspiration
- Dry, coarse, leathery skin; pale
- Poor circulation
- Coarse hair or hair loss
- Dry eyes – blurred vision
- Swelling or puffy eyelids
- Digestive problems, irritable bowel syndrome, or acid indigestion
- Constipation
- Headaches – moderate to severe
- Poor short term memory and concentration
- Arthritis, joint pains
- Low blood pressure
- High blood pressure
- High cholesterol or atherosclerosis
- Diabetes
- Hypoglycemia
- Low libido
- Anxiety – panic attacks
- Depression – moderate to severe
- Behavioral and emotional disorders
- Wounds that heal slowly
- Menstrual problems (include PMS or hysterectomy)
- Infertility
- Enlarged thyroid-goiter
- Acne
- Lateral halves of eyebrows missing
Figure 1: Hypothyroidism is a condition of insufficient output from the thyroid gland. Broda Barnes, M.D., Ph.D., (perhaps the most famous thyroid researcher and author of Hypothyroidism: The Unsuspected Illness), reports that the symptoms related to low thyroid vary widely and may include those shown in the table. Why not check all that apply to you?
References
- Barnes B, and Galton, L. Hypothyroidism, the Unsuspected Illness. 1972, Harper and Row, New York.
- Goldberg JB, Kurland AA. Dilantin treatment of hospitalized cultural-familial retardates. J Nerv Ment Dis. 1970 Feb;150(2):133-7.
- Daniel R. Psychiatric drug use and abuse in the aged. Geriatrics. 1970 Jan;25(1):144-5.
- Smith WL, Lowrey JB. Effects of diphenylhydantoin on mental abilities in the elderly. J Am Geriatr Soc. 1975 May;23(5):207-11.
- Kim D. Practical Use and Risk of Modafinil, a Novel Waking Drug. Environ Health Toxicol. 2012; 27.
Dear Dr Dean,
I read with interest your interview and your own personal smart drug regimen. I noted that you like to use modafinil for alertness and attention but that the cost puts you off. I concur! But have you ever used adrafinil, and if so, how do you see it comparing to modafinil?
Yes, I’ve used adrafinil, but do not find its effects quite as profound as those from modafinil or Nuvigil®. However, that may just be me. Others have told me that they have experienced virtually identical effects from adrafinil and modafinil, and prefer to use adrafinil due to its more reasonable pricing. It all seems to depend on ‘biochemical individuality.’
[Ed.- IAS provides adrafinil/ Adra-Pro™ and via www.modafinil-store.com the three major brands of modafinil, Alertec®, Modiodal® and Provigil®].
Dear Dr. Dean,
My wife suffers badly from restless legs syndrome? Do you have any suggestions for this exasperating, debilitating condition?
BMC, USA
A. Have her try Gabapentin, before bedtime. Gabapentin is a very effective nerve-stabilizer, and should give her a lot of relief. It is well-tested to alleviate restless legs.1-3
The key is the dosage. This can usually range from 300-1200 mg. Start with a low dose, and gradually titrate the dose to that which gives her relief, but does not leave her “hung over” in the morning. Gabapentin is a great sleep-promoter, which actually enhances slow-wave sleep.4
References:
- Happe S, Klösch G, Saletu B, Zeitlhofer J. Treatment of idiopathic restless legs syndrome (RLS) with gabapentin. Neurology. 2001 Nov 13;57(9):1717-9.
- Garcia-Borreguero D, Larrosa O, de la Llave Y, Verger K, Masramon X, Hernandez G. Treatment of restless legs syndrome with gabapentin: a double-blind, cross-over study. Neurology. 2002 Nov 26;59(10):1573-9.
- Adler CH. Treatment of restless legs syndrome with gabapentin. Clin Neuropharmacol. 1997 Apr;20(2):148-51.
- Lo HS, Yang CM, Lo HG, Lee CY, Ting H, Tzang BS. Treatment effects of gabapentin for primary insomnia. Clin Neuropharmacol. 2010 Mar-Apr;33(2):84-90.
- Nandy, K., Mostofsky, D.I., Idrobo, F., Blatt, L. and Nandy, S. Experimental manip[ulations of lipofuscin formation in aging mammals. In: Lipofuscin—1987: State of the Art. I. Zs. Nagy, Editor, pp. 289-304, Elsevier Science Publishers, Amsterdam, 1988
- Del Roso, A., De Tata, V., and Bergamini, E. Regional distribution of the age pigment accumulation across the free wall of the left ventricle of rat heart. In: Lipofuscin—1987: State of the Art. I. Zs. Nagy, Editor, pp. 441-442, Elsevier Science Publishers, Amsterdam, 1988.
- Nkontchou, G., Casson, E., Aout, M., et al. Impact of metformin on the prognosis of cirrhosis induced by viral hepatitis C in diabetic patients. J Clin Endocr Metab, 96: 2601-2608, 2011.
Doctor Dean,
We met about fifteen years ago. After a lecture you gave in a small auditorium at a Hotel/motel in Santa Clara, CA, I was the one who came up on stage and shook your hand before asking my question. I had already read your 1990 book, Smart Drugs & Nutrients, and thanked you for the service you had provided me and others. Today I have discovered that Hydergine has been discontinued Hydergine! Can you suggest an alternative product with similar purported benefit? I am retired and 67 years experienced. The supplements I consume are too many to list but I have tried one at a time beginning after reading Durk & Sandy’s book and then your books, too, and since 2003 I have taken one 800 mg Piracetam daily and one Hydergine on Monday, Wednesday, Friday and Saturday since 2005. The third regular item I purchase is centrophenoxine. Again, thank you so much for all the information you have given to me in books and the three cassette tape sets I have also purchased.
Dear Sir,
Yes, I remember the talk. You are correct that Novartis have discontinued Hydergine®. Fortunately, the IAS folks found a high-quality generic manufacturer, whose product they sell under the name Hy-Pro™. They also offer generic choices for Nootropil® (piracetam) as Pira-Pro™ and for Lucidril® (centrophenoxine/meclofenoxane) as Centro-Pro™. With these substitutions, you should be able to continue your “smart drug” program at a reduced cash outlay.
Ward Dean, MD
Dear Dr. Dean,
I recently heard a well-known antiaging physician say that he often sees rises in cortisol levels when a man consumes pregnenolone; as I use 100mg of pregnenolone regularly I find that rather disconcerting. May I ask you what has been your experience?
J.W., Washington
Dear JW,
As you can see from the accompanying figure 1, pregnenolone holds a premier position in the hormone cascade, and can be converted into virtually all of the steroid hormones, depending on the body’s needs (Fig. 1).
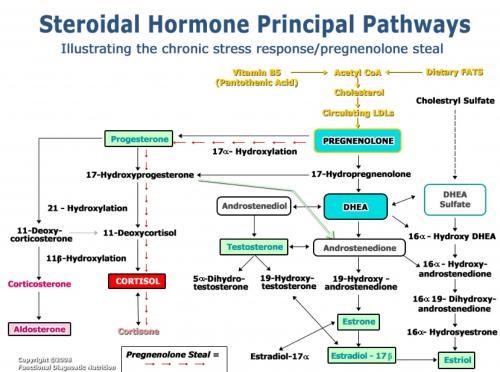
Figure 1: The hormone cascade starts with cholesterol and then pregnenolone.
The pathway has a “right side” and a “left side”. The right side includes pregnenolone > DHEA > Testosterone and the estrogens. The left side involves pregnenolone > progesterone > cortisol and progesterone > aldosterone.
During times of severe or prolonged stress, pregnenolone may be diverted from the right side of the pathway in order to feed the left side of the pathway, resulting in elevated cortisol in response to the stress. This is known as the “pregnenolone steal” syndrome, as shown at the bottom of figure 1. Consequently, DHEA production suffers because less pregnenolone is available for the right side of the pathway, throwing the cortisol/DHEA ratio out of balance.
The problem is not due to pregnenolone supplementation, but to the stress. If one’s cortisol is rising (due to stress), then I recommend continuing to take pregnenolone and balancing it with additional DHEA. This can restore a normal cortisol/DHEA balance, which will help the body to deal with the stress. Thus, it’s not the pregnenolone that’s driving the cortisol—it’s the stress. For example, in a recent study of the effect of pregnenolone on schizophrenia, doses of pregnenolone were titrated up to 500 mg/day for four weeks in 18 schizophrenics. Although treatment with pregnenolone resulted in fourfold elevation in serum levels of pregnenolone, tripled serum pregnenolone sulfate levels and increased the GABAergic neurosteroid allopregnanolone fivefold, plus DHEA-S levels by approximately 16%, treatment with pregnenolone did not increase serum testosterone, free testosterone, cortisol, DHEA, estradiol, or androstenedione levels. (1)
Pregnenolone, like DHEA, drops precipitously with increasing age (Fig. 2), and should be routinely supplemented. The usual dose in aging men and women is 25-50 mg per day, although more or less is commonly taken, based on individual need.
Figure 2: Age and sex differences of pregnenolone sulfate in the serum of 230 women aged 10–70 years (empty circles) and 179 men aged 4–79 years (solid circles). (2)
I hope this answers your question and relieves your stress.
References:
- Marx CE, Richard Keefe RSE, Robert W Buchanan RW, et al. Proof-of-Concept Trial with the Neurosteroid Pregnenolone Targeting Cognitive and Negative Symptoms in Schizophrenia. Neuropsychopharmacology. 2009; 34(8): 1885–1903. doi: 10.1038/npp.2009.26
- Havlíková H, Hill M, Hampl R, and Stárka L. Sex- and Age-Related Changes in Epitestosterone in Relation to Pregnenolone Sulfate and Testosterone in Normal Subjects. The Journal of Clinical Endocrinology & Metabolism. 2002;87(5): 1925–2413. DOI: http://dx.doi.org/10.1210/jcem.87.5.8499
Dear Dr. Dean,
I went and saw a sleep doctor and he prescribed trazodone 50 mg. It did nothing at 50 mg but at 75 mg it seemed to give me about 3 hours of sleep, in fact it felt a lot like Benadryl®. However, I am having great difficulty in sleeping and this minimal amount is making me feel like a basket case! Can you please make a suggestion that can improve my situation? M.W., California
Dear M.W.,
First, although I know that trazadone is commonly recommended by many physicians, I believe it is ineffective as a sleep inducer (a somnificant). I preferentially use Gabapentin (Neurontin) for insomnia.
Gabapentin is an analog of GHB (gamma-hydroxy-butyrate) and shares many of GHB’s sleep-inducing benefits. For example, it enhances sleep quality, increases slow wave sleep and decreases spontaneous arousal.(1) I suspect it enhances all four phases of sleep, as does GHB. Interestingly, there has been a review of gabapentin as a sleep-inducer, compared to trazadone.(2) Patients who received gabapentin improved significantly more than did patients who received trazodone, and gabapentin-treated patients were less likely than trazodone-treated patients to have initial insomnia and to awaken in the morning feeling tired and worn out. In my experience, gabapentin is effective for most people at a dose of 600-800 mg at bedtime. Some people are very sensitive and do well on even less; others are resistant and need higher doses (I have a few patients on 1800-2400 mg).
Fortunately, gabapentin does not interact adversely with other drugs, has few adverse side effects (sleepiness is the most common) and wears off rapidly (just like GHB), usually snapping people awake in the morning, without any hangover. Another advantage is that gabapentin is not a controlled drug like GHB.
Ward Dean, MD
References:
- Lo HS, Yang CM, Lo HG, Lee CY, Ting H, Tzang BS. Treatment effects of gabapentin for primary insomnia. Clin Neuropharmacol. 2010 Mar-Apr; 33(2):84-90.
- Karam-Hage M, and Kirk J. Brower KJ. Open pilot study of gabapentin versus trazodone to treat insomnia in alcoholic outpatients. Psychiatry and Clinical Neurosciences. 2003 October;57(5): 542–544. October 2003 DOI: 10.1046/j.1440-1819.2003.01161.
[Ed. – the brand name of gabapentin is Neurontin®]
Dear Dr Dean
I am a 58 year old woman who eats really well and exercises 5 days a week at a gym with weights cardio and ab exercises, for about 9 years. I have just finished an education degree and teach a couple of days per week.
I see an antiaging doctor in Melbourne and take Estradiol / estriol 50:50 6MG BI Gel daily with 0.5/ML testosterone. Progesterone 200mg capsules in the evening 25 days of the month with a rest of 5 days per month, I have been taking this for about 8 years.
I take Metformin 500mg tablets twice a day and for the past 4 months have been taking an antidepressant called Lovan 20 tab 1 per day. In 2000 I had half my thyroid removed because of tumours and have been swallowing thyroxine sodium tablets 100mcg per day ever since. I have blood tests and they are fine. I feel healthy and I am in good spirits and generally look years younger and stronger than anyone I know in my age group. However I have one major problem.
I have the “org” but not the “gasm”. It’s like my little button has switched itself off. Can you shed some light on this? I have read IAS articles. Would Russian peptides help me? If so, which ones specifically? Or should I try oxytocin?
I respect you so very much, Dr Dean. Perhaps when I teach in America I could see you for an appointment. Until then, have you some idea of where I should be looking to overcome this hormone imbalance?
J.C., Australia.
Dear JC
First, I noted that you not supplementing with either DHEA or Pregnenolone – both of which decline dramatically with age. However your physician is inexplicably prescribing testosterone for you – which will preclude your taking DHEA, because women very efficiently convert DHEA into testosterone. Taking both testosterone and DHEA would probably really throw you out of balance. I rarely prescribe testosterone to women, because they can almost always restore testosterone to youthful levels by taking DHEA. DHEA by itself is a well-documented mood elevator (1). I suggest you discontinue taking testosterone, and start taking DHEA – for women, 25mg is usually enough, (although you may need to adjust it slightly up or down), first thing in the morning.
Also, Pregnenolone is another over-looked hormone that declines with age, and which converts preferentially, and also to DHEA.
Notwithstanding the most likely cause of your anorgasmia may be your anti-depressant. Lovan (aka Prozac, fluoxetine) is a well-known cause of sexual dysfunction and loss of libido
I suggest weaning yourself from Lovan and switching to 5HTP, 150-300mg per day at bedtime on an empty stomach (2,3). 5-HTP is a precursor of serotonin and usually produces equal benefits of the SSRI’s, without the adverse effects.
Also you might consider Deprenyl, which has been best known as an “antiaging, life-extending aphrodisiac.” (4-7) Although most of the studies of the aphrodisiac effects of deprenyl have been conducted on male rats, the effect has generally been attributed to its MAO-B inhibiting effect, which is shared equally by both sexes. Another possible cause of deprenyl’s aphrodisiac effect may be to its less well-known ability to raise serum levels of Nitric Oxide (8,9) – to which the effects of Viagra and Cialis are attributed.
Deprenyl has also been shown to be an effective antidepressant, which you may find of additional benefit (10-17). Prof. Josef Knoll recommends those of us who are over 45 take 10-15mg Deprenyl per week (about 2mg/day) for its antiaging, neuroprotective effects (18).
Oxytocin as you suggested may also help – but I like to try the cheap stuff first.
Ward Dean, M.D.
References
- Barrett-Connor E., Von Muhle, D, Laughlin G, Kripke A. Endogenous levels of dehydroepiandrosterone sulfate, but not other sex hormones, are associated with depressed mood in older women. The Rancho Bernardo Study. J am Geriatr Soc 1999, 47(6), 685-691.
- Byerley W, et al. 5-Hydroxytryptophan: A Review of Its Antidepressant Efficacy and Adverse Effects. J Clin Psychopharmacol 1987; 7; 127-37.
- Poeldinger W, et al. A Functional-Dimensional Approach to Depression: Serotonin Deficiency as a Target Syndrome in a Comparison of 5-Hydroxytryptophan and Fluvoxamine. Psychopathology. 1991; 24; 53-81.
- Yen TT, Dallo J, Knoll J. The aphrodisiac effect of low doses of deprenyl in male rats. Pol J Pharmacol Pharm. 1982 Nov-Dec; 34 (5-6):303-8.
- Knoll J, Yen TT, Dallo J. Long-lasting, true aphrodisiac effect of (l)-deprenyl in sexually sluggish old male rats. Mod Probl Pharmacopsychiatry. 1983; 19:135-53.
- Dallo J, Yen TT, Knoll J. The aphrodisiac effect of deprenyl in male rats. Acta Physiol Hung. 1990;75 Suppl:75-6
- Ruehl WW, Entriken TL, Muggenburg BA, Bruyette DS, Griffith WC, Hahn FF. Treatment with L-deprenyl prolongs life in elderly dogs. Life Sci. 1997; 61(11):1037-44
- Thomas T, McLendon C, Thomas G. L-Deprenyl: nitric oxide production and dilation of cerebral blood vessels. Neuroreport. 1998 Aug 3;9(11):2595-600
- Thomas T. Monoamine oxidase-B inhibitors in the treatment of Alzheimer’s disease. Neurobiol Aging. 2000 Mar-Apr; 21(2):343-8
- Lee KC, Chen JJ. Transdermal selegiline for the treatment of major depressive disorder. Neuropsychiatr Dis Treat. 2007;3(5):527-37
- Feiger AD, Rickels K, Rynn MZ, Zimbroff DL, Robinson DS. Selegiline transdermal system for the treatment of major depressive disorder: an 8-week, double-blind, placebo controlled, flexible-dose titration trial. J Clin Psychiatry. 2006 Sep;67(9):1354-61
- Amsterdam JD. A double-blind, placebo controlled trial of the safety and efficacy of selegiline transdermal system without dietary restrictions in patients with major depressive disorder. J Clin Psychiatry. 2003 Feb;64(2):208-14
- Higuchi H, Kamata M, Sugawara Y, Yoshida K. Remarkable effect of selegiline (L-deprenyl), a selective monoamine oxidase type-B inhibitor, in a patient with severe refractory depression: a case report. Clin Neuopharmacol. 2005 Jul-Aug;28(4):191-2
- Amsterdam JD, Bodkin JA. Selegiline transdermal system in the prevention of relapse of major depressive disorder: a 52-week, double-blind, placebo-substitution, parallel-group clinical trial. J Clin Psychopharmacol. 2006 Dec;26(6):579-86
- Sunderland T, Cohen RM, Molchan S, Lawlor BA, Mellow AM, Newhouse PA, Tariot PN, Mueller EA, Murphy DL. High-dose selegiline in treatment-resistant older depressive patients. Arch Gen Psychiatry. 1994 Aug;51(8):607-15
- Kitaichi Y, Inoue T, Mitsui N, Nakagawa S, Kameyama R, Hayashishita Y, Shiga T, Kusumi I, Koyama T. Selegiline remarkably improved stage 5 treatment-resistant major depressive disorder: a case report. Neuropsychiatr Dis Treat. 2013;9:1591-4. Doi: 10.2147/NDT.S49261
- Higuchi H, Kamata M, Sugawara Y, Yoshida K. Remarkable effect of selegiline (L-deprenyl), a selective monoamine oxidase type-B inhibitor, in a patient with severe refractory depression: a case report. Clin Neuropharmacol. 2005 Jul-Aug;28(4):191-2
- Knoll J. Deprenyl-medication: a strategy to modulate the age-related decline of the striatal dopaminergic system. J Am Geriatr Soc. 1992 Aug;40(8):839-47.
Dear Dr Dean
I have knots in my legs that are painful at night. I also have painful upper arms. My chiropractor and podiatrist have suggested that I have tendonitis, but my primary care doctor has not made a diagnosis or prescribed a medication. I have been taking a homeopathic supplement for tendons at bedtime. Sometimes, it is affective but some nights, it doesn’t help.
The tenderness in my legs is on the outside of my calf and thigh and occasionally in my right hip joint. What would you recommend to eliminate the discomfort in my legs, which becomes more painful during the hours of the night? D.S. USA
Dear DS
What you are describing doesn’t sound like tendonitis to me. Tendonitis is an inflammation or irritation of a tendon, a thick cord that attaches bone to muscle, and thus occurs nears the site of insertion of the tendon, near a joint, not in the locations you describe. I think you are suffering from a variant of the Restless Leg Syndrome (RLS), and you should respond favourably o the same recommendation as above.
Natural remedies for RLS include increasing your intake of potassium and magnesium – two minerals which are commonly deficient in those with RLS. Magnesium is a natural muscle relaxer – which explains bathing in Epsom salts (magnesium sulfate) is so relaxing. I suggest a teaspoon of Morton’s Lite Salt each day (Lite Salt contains 320mg sodium, and 340mg potassium per ¼ teaspoon) and magnesium to bowel tolerance (you can’t OD on magnesium, because it will cause diarrhoea.