The epidemic of low thyroid diseases
The function of every cell in the body depends on the presence of an adequate amount of thyroid hormones in order to do the work it is supposed to do. Brain cells need thyroid hormones to think. Muscle cells need thyroid hormones to move.
Therefore, what happens when a person’s thyroid is not working as well as it should? When inadequate amounts of thyroid hormones are able to enter into each cell to perform its normal work, what does a person experience?
There is this magnificent little molecule called T3 (one of several thyroid hormones), that is absolutely necessary for the cells of the body to produce energy. You eat food and you breathe in oxygen–but if you don’t have adequate T3, the food and the oxygen won’t be able to do much. T3 is involved in the process of mating food and oxygen (what you eat and what you breathe) in order to make energy for muscles, nerves, and other cells so that they are able to do what they are supposed to do.
Imagine that your muscles don’t have enough thyroid hormone. What are you going to experience? The muscles might feel tired and weak. And they might hurt. If your brain is deficient in thyroid hormones, it might seem as though your brain isn’t working. As some of my patients describe it, “My brain feels like it’s in a fog”. It’s hard to think. Your joints might swell and hurt if thyroid hormones are not getting into the cells where the hormones can do their work. Your ovaries may not work properly and you can’t get pregnant (this is a fairly common issue, often undiagnosable using only conventional testing). Your intestines might not have the energy to function and you experience constipation–or paradoxically, you might have diarrhea. It’s well known that low thyroid causes hardening of the arteries (atherosclerosis) which leads to heart attacks and strokes. We’ll explore this further later in the article.
In addition to the above, low thyroid is a common cause of many symptoms including high cholesterol levels, premenstrual syndrome, post-partum (after having a baby) depression, weight gain, depression, cold extremities, chronic fatigue syndrome, fibromyalgia, high levels of homocysteine (a natural material in the blood, but large amounts can be dangerous), high blood pressure, and diabetes.
Do you happen to know anyone with any of those problems? Of course, we all do. And there is a crowd of people out there with these types of problems.
Can you trust the accuracy of the routine thyroid tests?
A low thyroid status can cause the problems listed above. But many people with those problems have been told that their thyroid is normal. Is it always true that their thyroid is, in fact, “normal?”
A question we should ask is this: Might a lot of those symptoms or diseases be caused primarily or in part by low thyroid status but missed due to conventional testing and diagnostic methods? What is particularly interesting is that many of these problems will tend to improve or disappear when there is appropriate thyroid treatment.
Because there are so many people with fatigue, menstrual disorders, high cholesterol, depression, diabetes and such that are able to enjoy a much higher level of function with appropriately prescribed thyroid therapy, many doctors are recognizing that we are facing an epidemic of hypothyroidism (low thyroid status) that is not adequately diagnosed by using only blood tests during a medical workup.
These physicians are beginning to realize that the currently popular method of testing for thyroid status is inadequate, and often falsely leads doctors to believe that their patients have sufficient thyroid hormones when, in fact, they do not.
When we understand 1) what the thyroid hormones do, and 2) what it looks like when the thyroid system is not working properly, we are better able to accurately determine thyroid status than by looking only at a laboratory test or two.
We’ll try to explain this so that it isn’t too confusing. But first let’s consider the potential benefits of having a thyroid status that is slightly on the higher side of normal rather than slightly on the lower side of midrange.
Was Mona Lisa hyperthyroid?
Allow me to quote a Nobel Prize winner, Harvard cardiologist Dr. Bernard Lown, addressing this issue in a tangential way. Dr. Lown deeply admired his chief mentor, Dr. Samuel Levine, and wrote about him in a wonderful book, The Art of Healing. His affection for this brilliant doctor brightens the paragraphs and pages in which he eulogizes this wise gentleman.
After Dr. Levine retired, he began seeing Dr. Lown as his personal cardiologist. Through the roles of student and doctor, Dr. Lown learned a great deal about Dr. Levine. Perhaps the most interesting observation regarding Dr. Levine, in the current context, is the following:
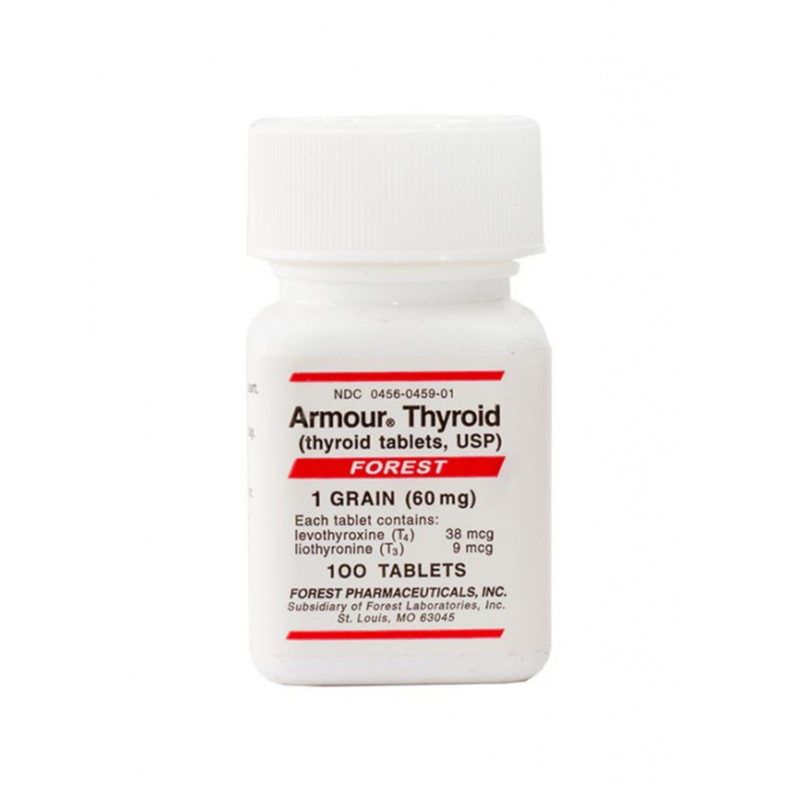
“Dr. Levine was impressed with the brightness and quickness of hyperthyroid (too much thyroid) patients. He admired them intensely, and believed that the condition protected them against coronary artery disease. I later learned, when he became my patient, that he had taken three grains of thyroid daily (that is, Armour® thyroid or equivalent) for more than thirty years. He maintained that those with increased thyroid function had bright, sparkling eyes and appeared to be interesting people, because personality is conveyed largely through the eyes. Levine suggested that the universal fascination with the Mona Lisa stems from her being hyperthyroid. He insisted that a slight stare makes viewers believe that she is focusing on them and is the basis for the attention this painting has received over the centuries.”[i]
Dr. Levine is here talking about people with a slight excess of thyroid by current standards, not severely hyperthyroid people. Because he would rather be slightly hyperthyroid than slightly hypothyroid (low thyroid), Dr. Levine took a rather generous dose of natural, desiccated thyroid for many years.
Whether the good doctor was correct in his appraisal of Mona Lisa, we’ll never know. But in regard to other issues, Dr. Levine is increasingly being shown to be correct. Namely, the benefit of thyroid for the cardiovascular system, the use of natural, desiccated thyroid, and the value of dosing a patient toward the upper end of the acceptable range rather the low end.
It may help to know what is meant by natural, desiccated thyroid. In the marketplace, it is often known as Armour® thyroid, Nature® throid or ERFA®.
Poor lifestyle and hypothyroid symptoms
In light of this information, how do you take action if you think that you might have low thyroid function? A couple of cautions you should consider before concluding that you must have hypothyroidism.
First, diet is terribly important. Putting on weight while drinking Frappuccino’s in the morning and a few pints in the evening is not likely a thyroid problem.
Second, if you’re tired but you’re working three jobs, sleeping 4-5 hours each night, and getting no exercise, I doubt that your fatigue is primarily a thyroid issue.
Lifestyle choices are hugely important for feeling good and having plenty of energy. If you really want to feel good, pay attention to your food choices, sleep habits, exercise and other important lifestyle issues.
But if you are treating your body well, feeding it well, and you’re still feeling poorly, thyroid legitimately might be an important factor in your getting well.
The TSH test: measuring the voice of the pituitary
This is where some of the challenge for the consumer (you) comes in. If you’re concerned, legitimately, about some of these thyroid related issues, how do you know if you need thyroid? Without getting very technical, there are a few basic definitions that you need to have a handle on in order to understand what your lab work means and how to discuss your situation with your doctor.
The most frequent way that doctors evaluate thyroid status is to have blood drawn in which the thyroid stimulating hormone (TSH) is checked. You especially need to understand the significance of the TSH.
The pituitary is a small gland situated in the forward part of the head a bit behind and between the back ends of the eyes. It’s the boss of the thyroid. The pituitary tells the thyroid what to do. The pituitary continuously samples the blood for one of the thyroid hormones and if the thyroid is not doing its job, the pituitary says, “Get to work.” At first it suggests the need for improved efficiency on the job with a very soft voice (TSH is not elevated). But if there is an inadequate response on the part of the thyroid, the pituitary raises its voice bit by bit until it can be shouting and even screaming at the thyroid to get off its duff and start producing thyroid hormones, (elevated TSH).
The current definition of low thyroid primarily has to do with how loudly the pituitary is talking to the thyroid. As long as the pituitary’s voice is not too high, it is assumed that the thyroid is doing its job. After all, the pituitary, which monitors and bosses the thyroid, is happy, or so the current medical thinking goes. If the pituitary is raising its voice (elevated TSH), then the thyroid must not be producing adequate thyroid hormones. A person with a pituitary having to shout (elevated TSH) at the thyroid, is by current popular definition hypothyroid.
The TSH is the measure of the how loudly the pituitary is speaking or shouting. The conventional definition for low thyroid function (hypothyroidism) is a TSH over about 5.00. So if you go to the doctor and your TSH is 5.20 you might be told that your thyroid is a bit low and you need to begin thyroid therapy. On the other hand, your TSH might be 4.80. In which case your doctor might say your thyroid is normal and you don’t need any thyroid.
Typically unrecognized limitations in using the TSH test
There are several problems with this definition. First and foremost has to do with the clinical picture of what is happening with you. Do you have any signs or symptoms of low thyroid? If you do have symptoms/signs that are suspicious for low thyroid, then a TSH of 4.80 or even a lot lower might be consistent with low thyroid.
As one example, suppose that the pituitary is “hoarse” or has “laryngitis”. It can’t raise its voice even if it wants to. It might be trying to scream but only getting out a gentle whisper. In which case, a low thyroid would be consistent with a low TSH (contrary to the usual picture). So we either have to test for “pituitary laryngitis” (which can be done) or pay close attention to the signs and symptoms of the person.
Often a woman will have a damaged pituitary following childbirth in which it becomes unable to raise its voice (Sheehan’s syndrome). These women are often misdiagnosed as depressed or malingerers when, in reality, they are hypothyroid with low TSH. Treat them with thyroid as they should be treated and all becomes well. This is one of the challenges of an overly-simplistic diagnostic approach.
Another reason that total reliance on TSH levels is inappropriate is that TSH levels can vary substantially during the day. There can easily be a 200% or more variance during the day in a given individual. On the desk in front of me are the 24-hour measurements of two patients where the TSH was drawn every few minutes. With one patient the 24-hour low was about 0.30 and the high was about 2.00. The other showed a low of about 1.00 and a high during the 24 hours of approximately 5.00.[ii]
A TSH of 1.00 is considered good, but a TSH of 5.00 would often be considered high, indicating low thyroid status. So which is the TSH to use?
Another legitimate and argued question is: At what level is the TSH too high? As mentioned above, most labs use a number in the vicinity of 5.00. The American Society of Clinical Endocrinologists suggests that when treating low thyroid problems the TSH should be kept below 3.00.[iii] If a TSH above 3.00 is not best for a patient being treated, it’s reasonable to ask if a TSH of 5.00 might not be too high for an untreated person.
The experts in designing tests to evaluate human health are members of the National Academy of Clinical Biochemistry. They have recently noted the following:[iv]
- Over 95% of healthy people with optimal thyroid function have a TSH that is less than 2.50.
- Patients with a TSH above 2.50 may be in the early stages of thyroid failure.
- When treating a patient, the TSH optimally should not be above 2.00.
It is also important to measure the actual amount of thyroid hormones present in the blood. There are two main hormones. One is called T4, as it is the thyroid hormone with four iodine atoms attached to it. The other is T3, because it has three iodine atoms attached. T3 is some three to ten times as active as T4. If T4 or T3 are low, (or even low end of normal range) the thyroid system may not be functioning optimally.
One other thing; if you have an inflammation of the thyroid gland (thyroiditis or Hashimoto’s thyroiditis) you can have normal levels of TSH, T4 and T3, but the whole thyroid system might not be working right. Often we find that people with thyroiditis feel much better when treated with thyroid hormones.
Thus we see that measuring only TSH levels is inadequate to optimally evaluate the thyroid status. We believe that a thorough initial evaluation should include TSH, thyroid antibodies (to check for thyroiditis), free T3 and free T4 (the active or available forms of T3 and T4) and possibly reverse T3.
A better way to diagnose low thyroid
Ultimately, the most important factor in making a diagnosis is the knowledge and awareness of the physician. A physician aware of the importance of optimal thyroid function is going to consider at least the following factors:
- Your blood work.
- Your history including important symptoms you are experiencing.
- An endocrinologically oriented physical examination.
- Your temperatures (thyroid maintains body heat).
For a variety of reasons that we will not discuss in any detail here, every blood test may be perfectly normal and a person might still need thyroid hormone supplementation. That’s the reason for the four-point approach to evaluation.
If we return to the thinking of the previously-referenced Dr. Samuel Levine, you’ll appreciate what I mean. Dr. Lown says the following about his mentor:
“He recognized… that ‘medicine is the science of uncertainty, the art of probability.’ He believed that the bulk of relevant information could be obtained from a properly gathered history and meticulously executed physical examination. He taught that a battery of tests must not replace a mind willing to think… “He hinted that frequent reliance on a so-called workup, engaging the heavy medical artillery of the day, such as X-ray or cardiac fluoroscopy, electrocardiography, phonocardiography, blood work and urine analysis, is testimony to a lack of clinical skill…”[v]
My own mentor on the subject of thyroid evaluation and treatment was Broda Barnes, M.D., Ph.D. Dr. Barnes was direct in his thoughts regarding the evaluation and treatment of patients. He said, with great vigor; “Always treat the patient, not numbers on paper.”[vi] By this he meant that many doctors are too busy to listen to the patient and to do the requisite exam, or they were ignorant of what the signs and symptoms of low thyroid truly were. Thus, hypothyroidism was, to them, only what the numbers on paper would report. If a patient’s TSH was 4.80, in these doctors’ minds the patient was normal. If the TSH was 5.20, the patient was hypothyroid. For Dr. Barnes, that was not being a good physician.
A brief review to clarify
1. TSH is the generally accepted method of diagnosing thyroid status. A high TSH is thought to always indicate low thyroid status. A low TSH is usually interpreted as too much thyroid. And a normal TSH is considered indicative of normal thyroid function.
2. There is now a large body of data that shows us that this interpretation of TSH is only legitimate in some cases. People who are depressed may have standard laboratory tests all showing normal. But they are often shown to be hypothyroid when more advanced testing is done. People with inflammatory diseases such as some forms of arthritis will often have normal standard lab reports–but when more accurate testing is done they are shown to be low in thyroid. Ditto, when one is dieting (calorie restriction). Ditto with chronic fatigue syndrome. Ditto with diabetes and fibromyalgia and obesity and others.
3. The best way to diagnose thyroid status is to use a combination of:
a. A variety of blood tests, not just TSH, or TSH and free T4.
b. A thorough history taken by someone who understands nuances of hypothyroid manifestations.
c. An endocrinologically oriented physical exam.
d. Basal body temperatures or other methods of evaluating metabolic status.
Dr. Ord in London
A correct diagnosis of thyroid status may be critically important. Let’s use the example of atherosclerotic heart disease (heart attacks).
In the mid-1870s, virtually nothing was known about the function of the thyroid. One of the classic presentations in the history of thyroid research was given by Dr. William Ord. He described a patient who had been a healthy and industrious woman at the age of 49. She gradually became cold, experiencing shivering spells. Her mental faculties and memory decreased. Her movements became slow and awkward–it required two hours for her to dress herself. She would fall asleep unless she was moving. She died at age 60.
On autopsy it was discovered that her thyroid gland was entirely destroyed by fibrous tissue. The pathologist described the vascular system like this: “…the arteries were everywhere thickened, the larger ones atheromatous.”
In other words, she had extensive atherosclerotic (hardening of the arteries) disease of all larger arteries. Dr. Ord was convinced that there was a connection between the destruction of the thyroid gland and the symptoms she had, including the damage to the arteries. A commission was chartered to explore the function of the thyroid gland. Over the following years, a reasonably clear picture of the role of the thyroid was obtained. What is clear and generally accepted is that low thyroid function causes or contributes to hardening of the arteries.[vii]
Professor Billroth of Vienna
This gentleman is one of the most famous surgeons of history. Very large goiters (enlarged thyroid glands) used to be relatively common. Cosmetically, they were disturbing. The good professor developed a safe and effective method of removing thyroid glands. However, with no thyroid gland remaining, the people became severely hypothyroid and would die of myxedema, a technical term for the swelling associated with very low thyroid function.
An Austrian law mandated that everyone dying in hospital be autopsied. It was discovered that all of these patients dying of low thyroid because their thyroids had been removed had generalized, severe hardening of the arteries throughout the body.
A student of Billroth, von Eilsberg, did further research demonstrating that the removal of the thyroid gland from sheep and goats led to systemic atherosclerosis.
Professors Pick and Pineless, also of Vienna, removed the thyroid glands of sheep and goats, but provided the animals with thyroid replacement similar to Armour® thyroid. These animals did not develop atherosclerosis.
American Research
Dr. Hurxthal of the Lahey Clinic in Boston reported on observations in their clinic. They would remove the thyroid gland of patients who were hyperthyroid (too much thyroid). Dr. Hurxthal noted that these patients would often have cholesterol levels that were quite low prior to the surgery. But after the surgery, if too much thyroid tissue were removed rendering the patient hypothyroid, they would often develop high levels of cholesterol.
The relationship between thyroid status and high cholesterol levels was so significant that Hurxthal suggested that serum cholesterol might be considered as a diagnostic measure for thyroid function. He even suggested that elevated cholesterol might be an indication for thyroid therapy if another cause for the hypercholesterolemia could not be found.[viii]
Professor William Kountz, Washington University of St Louis, published in 1951 Thyroid Function and Its Possible role in Vascular Degeneration. He reports on a study of patients with low body temperatures and many with elevated cholesterol. The first group was businessmen with an average age of 55. This group had little evidence of hardening of the arteries and the men were patients in his private practice. A second group were outpatients at the University Clinic. These men averaged age 61. Many already had evidence of some hardening of the arteries.
Each group was divided into two. One of the subgroups received thyroid treatment. The other subgroup did not receive thyroid. All groups were followed for five years and monitored for heart attacks and strokes.
· Group one: There were no deaths in those treated with thyroid. In the untreated group, 15% had a fatal heart attack or stroke.
· Group two: There was 3% mortality in the treated group and 19% mortality in the untreated group. Over six times as many men died in the untreated group.
Dr. Barnes went to Graz, Austria every year for fifteen years and spent at least one month studying the autopsy records accumulated over some 200 years. As mentioned above, every hospital death required autopsy.
The conclusion of a huge amount of work and research is this: Low thyroid people are subject to increased risk of infection and poorer ability to fight the infection. Prior to the advent of antibiotics these people would routinely die of infections prior to dying of heart attacks. The records show that those dying of infections had extensive hardening of the arteries. After antibiotics became available, these people would be treated allowing them to live long enough for heart attacks to kill them.
‘Normal’ vs. optimal
Recent research indicates that just having normal thyroid function based on TSH levels is not necessarily optimal. The increased risk of atherosclerosis in borderline hypothyroidism extends into the normal range. In other words, having a high normal TSH (borderline low function) increases your risk of hardening of the arteries. One study suggests that the lowest possible TSH within the normal range (i.e. around 0.4) is the best way to reduce risk of cardiovascular disease.[ix] “Normal” is not the same thing as optimal as this study demonstrates. In the field of antiaging or integrative medicine, our goal is to achieve the optimal range, not just the ‘normal’. Studies like this confirm our setting of higher goals.
Thyroid and cholesterol
People with subclinical hypothyroidism, (a technical term for people with no dramatic symptoms of low thyroid function and an elevated TSH) often have elevated cholesterol levels. When treated with thyroid replacement hormones, there is a significant decrease in both total cholesterol and in LDL (the so-called ‘bad’ cholesterol).[x]
The higher your T3 levels are, the lower your cholesterol levels are likely to be.[xi]
Another study looked at 35 male patients with severe atherosclerosis. They monitored these men for two years and again evaluated the amount of hardening of the arteries. In 14 there was no progression of the disease. 21 had significant progression. They then asked what was most significant in apparently preventing progression. One of the two most important factors was the T3 level, (the active form of the thyroid hormone included in Armour® thyroid but not in Synthroid® or its equivalents).[xii]
Articles like these begin to delve into the issue of which is the best way of treating low thyroid function. We’ll address this a little later. But with information such as this, many of us who work daily in this field question the notion of treating patients only with T4-containing preparations such as Synthroid® and Levoxyl®. This article shows that higher levels of T3 are at least suggestive evidence that a combination of T4 and T3 might be preferable to T3 only.
There are a large number of articles dealing with the issue of atherosclerosis and thyroid function. The challenge for a writer is choosing from so many that demonstrate the same principle: adequate treatment with thyroid hormones is often protective against hardening of the arteries and thus heart attacks.
Other benefits of appropriate thyroid replacement
Homocysteine is a known risk factor for heart attacks, strokes and peripheral artery disease like claudication (pain in legs with walking due to atherosclerosis).[xiii] It is a toxic metabolite (breakdown product) of the amino acid methionine. Elevated homocysteine levels are also associated with increased risk of bone fracture, dementia and attention deficit.[xiv]
People with low thyroid function tend to have high levels of homocysteine. People with high thyroid levels have low homocysteine levels. Therefore, treating people with high homocysteine levels and indications of hypothyroidism with appropriate thyroid therapy might benefit the high levels of homocysteine. This might reduce the risk of heart attacks, strokes and bone fractures.[xv]
Fatigue, sadness, irritability, anger, sleepiness, sense of being chilly or hot and a variety of other symptoms are rather common in today’s world. These are all possible signs of hypothyroidism.
A study published in 1999 looked at a group of patients who had previously been diagnosed with hypothyroidism. These patients had all been treated with T4 only (i.e. Synthroid® or an equivalent). However, their symptoms (as listed in the previous paragraph) had not improved.
The study reduced the amount of T4 given to each patient and added in a roughly biological equivalent of T3. These patients were now receiving a combination of T3 and T4 (similar to what one receives by using Armour® thyroid).
The conclusion of the study was that nobody did better on T4 alone. Most of the patients did better on the combination of T4 and T3. “It seems clear that treatment with thyroxine (T4) plus triiodothyronine (T3) improved the quality of life for most patients.”[xvi]
The best treatment for hypothyroidism
The most common therapy for hypothyroidism is T4 only, or a medication like Synthroid®, Levoxyl® or the generic levothyroxine. We have quoted various articles which suggest that the combination of T3 with T4 might be beneficial for a number of reasons. Dr. Levine, mentioned in the first part of this article, routinely took a combination of T3 and T4, the combination included in desiccated thyroid.
Dr. Barnes, my mentor on thyroid treatment, tested a variety of thyroid preparations. His conclusion was that most patients do best using Armour® thyroid.
Most important to me as a treating physician is: How does my patient feel with the treatment I’m providing? Does s/he feel better as a result of taking the thyroid hormone?
In the Bunevicius study reviewed above, patients taking T3 and T4 clearly felt much better than when they took T4 only.
My experience in treating patients like this for some 25 years is that most of them feel better taking the T3 and T4 combination than if they take the T4 alone. I’m not dogmatic about the use of the combination as I’m interested in the well-being of the patient. There are a few (very few) that actually feel better taking the T4 alone. For them I gladly prescribe Synthroid® or an equivalent.
Most patients, however, feel best taking the combination of T3 and T4. I routinely prescribe Armour® thyroid, which is desiccated (dried) thyroid tissue with a carefully regulated amount of T3 and T4 included in it.
How I transfer my patients from T4 only therapy to desiccated thyroid
One must first understand that there is not an exact equivalence between T4 preparations and Armour® thyroid. When a person takes T4 medications, the amount is given in micrograms. Synthroid® 50 means 50 micrograms of Synthroid®.
Armour® thyroid is given in milligrams and indicates the amount of desiccated (dried) thyroid tissue being used. The amount of T4 and T3 in the thyroid tissue is carefully regulated. One grain of Armour® thyroid contains 38 micrograms of T4 and 9 micrograms of T3. (Of interest, Armour® thyroid also contains T2 which has an increasing amount of fascinating data showing that it may also be an important factor in overall thyroid health. Synthroid®, of course, contains no T2.)
T3 is typically considered to be 4 times as potent as T4. One grain of Armour® has 38 micrograms of T4 plus 9 micrograms of T3, which is considered to be equal to approximately (4×9=36) 36 micrograms of T4. One grain of Armour® has the equivalence of 74 (38 mcg from T4 + 36 mcg equivalence from T3) micrograms of T4.
When I make the switch from Synthroid® to Armour® equivalents, I calculate approximately what the appropriate conversion would be. If a person is taking 75 micrograms of Synthroid®, I would consider changing to Armour® 60 mg based on the above calculations. If a person is taking 150 micrograms of Synthroid®, 120 milligrams of Armour® might be a good dose to change to.
I usually do not have them stop Synthroid® one day and start full dose Armour® the next day. I’ve found that I have fewer problems in making the conversion if a person takes half their Synthroid® dose and half their projected Armour® dose for 7-10 days. Then I have them stop the Synthroid® and take the full dose of Armour®.
Synthroid® equivalents are usually scored so they are easily broken in half. Armour® is not quite so easily divided, but is not too difficult with the use of a sharp knife. [Ed. – natural thyroids are available in a wide range of doses, so at least initially the patient can use a different dose before reaching their regular plateau].
The transitions are not always so clear cut. What to do when a person is taking 100 micrograms of Synthroid? I will usually transition to Armour® 90 milligrams, especially if I think that the person is running a bit low. Effectively, 90 milligrams of Armour® is a higher dose than 100 micrograms of Synthroid®. When making the change, I always let my patients know what to expect if it turns out they are getting too much thyroid. Typical symptoms of too much thyroid will be:
1. Rapid heart rate.
2. Palpitations.
3. Feeling hyper, something similar to drinking too much coffee.
If one of my patients begins having these symptoms, I advise them to stop the thyroid for a day or two and call my office for advice on dosing. We then will decrease the prescription appropriately. In practice, this seldom happens.
Conclusion
Optimal supplementation with natural forms of thyroid hormones has a strong healing benefit for those whose native thyroid status is less than optimal. When treatment is adequate it can help to lower cholesterol, improve depression and prevent advancement of atherosclerosis. It can also help to lower blood pressure and generally help people to feel better. There are many other benefits we are unable to discuss in a brief article.
The diagnosis of low thyroid function is based on a combination of the symptoms a person is experiencing, a physical examination, body temperatures and blood work. Most people will feel best if thyroid replacement is done using desiccated thyroid, which includes a combination of T3 and T4.
The information prese