Natural Antibiotic Alternatives: What You Need to Know
Antibiotic resistance is one of the most significant public health threats facing the population; this occurs when bacteria evolve mechanisms to withstand the drugs designed to kill them, rendering antibiotics less effective or, in some cases, completely useless.
When antibiotics were first discovered in the 19th century, they were heralded as the solution to life threatening bacterial infections such as pneumonia, strep throat, tuberculosis, wound infections, postpartum infections and more – in fact, they still are, and there’s no denying that antibiotics such as penicillin or amoxicillin have drastically changed modern medicine. However, antimicrobial resistance to antibiotics has led to changes in the way doctors view and prescribe them, on the basis that antibiotic resistance can undermine their safety and success.
What is antibiotic resistance?
Antibiotic resistance takes place when bacteria becomes less responsive to antibiotic compounds – this is due to the bacteria evolving to survive exposure. This can also happen if susceptible bacteria are killed by antibiotics but resistant bacteria is not; this resistant bacteria multiplies to become the predominant type and when antibiotics are administered, they are not as effective (or effective at all).
As the population increases, so does the spread of infection and disease. Over time, antibiotic resistance has increased to the point where medical professionals are actively prescribing antibiotics less even when bacterial infections may be present, to slow down the rate of resistance. This is of course at the discretion of the doctor in question, and it is important to still consult with healthcare professionals if you feel you need medication.
What causes it?
There are a number of reasons why this may happen including:
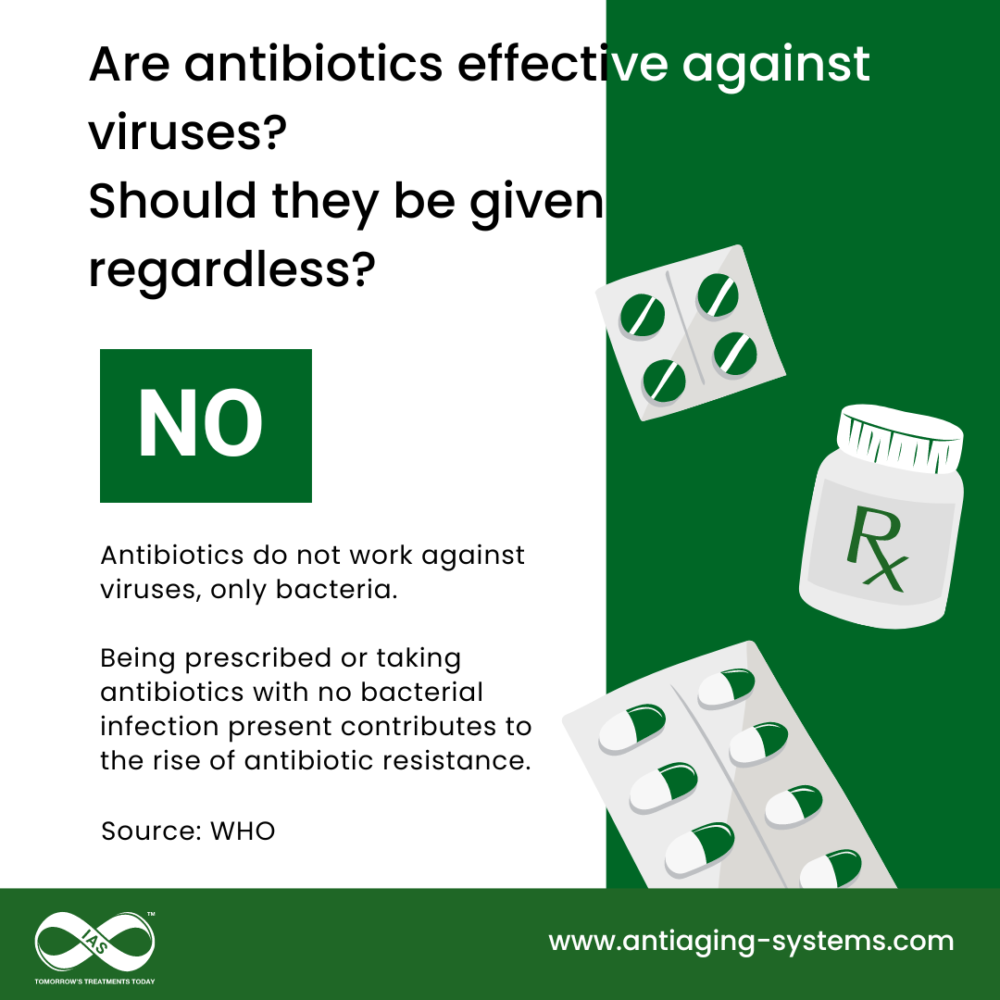
- Overuse and misuse – if antibiotics are given for viral infections, which they will not have an effect on, resistance may develop. In addition, if excessive amounts of antibiotics are prescribed, the bacteria in question has more chance to build up resistance.
- DNA exchange – bacteria can exchange DNA with other bacteria, which can cause resistance to pass around to unrelated species.
- Spread of infection – infectious resistant bacteria can spread between patients, increasing their resistance to antibiotics.
Key Health Implications
If the population continues to take antibiotics that work less effectively than in previous years, this can lead to a number of health concerns:
- Increased Infections
- Infections that were once easily treatable with antibiotics—such as UTIs, pneumonia, and skin infections—become more difficult to cure.
- This can lead to increased risk of hospital stays or longer hospital stays, more severe illness, and a greater risk of premature death.
- Surgical and Medical Procedure Risks
- Many routine medical procedures, such as surgeries, cancer treatments, and organ transplants, rely on antibiotics to prevent or treat infections. If antibiotics are not as effective as they need to be, this can lead to severe illness, longer recovery times and death.
- The Spread of Superbugs
- “Superbugs” are strains of bacteria that have become resistant to multiple antibiotics. These dangerous pathogens are harder to control and spread more easily within healthcare settings, communities, and even globally.
- The World Health Organization (WHO) and Centers for Disease Control and Prevention (CDC) have warned about the growing threat of superbugs, including Methicillin-resistant Staphylococcus aureus (MRSA) and drug-resistant tuberculosis (TB).
- Limited Treatment Options:
- With fewer antibiotics that remain highly effective against resistant bacteria, healthcare providers can face difficulties in finding treatments for even the most common infections. This limits the ability to control outbreaks and threatens the effectiveness of life-saving treatments.
The Fight Against Antibiotic Resistance
As above, one way that the healthcare sector is working to combat antibiotic resistance is to prescribe antibiotics less than in previous years, when absolutely necessary. Other solutions include:
- Completing Antibiotic Courses: Ensuring patients complete their full course of treatment, as partial courses can increase resistance.
- Developing New Antibiotics: Ongoing research into new classes of antibiotics is essential.
- Natural and Alternative Solutions: As interest grows in natural remedies, exploring complementary and alternative therapies, such as natural antibiotics, may reduce dependency on pharmaceutical antibiotics.
Natural Antibiotic Options
There are a number of natural antibiotic alternatives, some of which are readily available in our local store. These include:
- Honey (especially Manuka Honey): Known for its antibacterial properties and historical use in wound healing.
- Garlic: Contains allicin, a compound with strong antibacterial and antiviral effects.
- Oregano Oil: Rich in carvacrol and thymol, known for fighting bacterial infections.
- Echinacea: Popular for its immune-boosting and antibacterial qualities.
- Coconut Oil: Its medium-chain fatty acids, like lauric acid, have antimicrobial effects.
- Turmeric: Contains curcumin, which has potent antibacterial and anti-inflammatory properties.
- Thiocyanates ions supplements – these are produced naturally in the body and fight unwanted bacteria, fungi, yeasts and viruses. They do not attack healthy bacteria in the body and therefore do not weaken the immune system.
Taking natural antibiotic supplements or products offers a lower risk of creating resistant bacterial strains with fewer side effects compared to pharmaceutical antibiotics. They can also be used preventatively to boost the immune system with the goal of being ill less.
It is important to bear in mind that natural antibiotics are not a complete substitute for conventional antibiotics in severe cases and it is key to discuss any health concerns with a doctor or medical consultant if natural options are seeming not to help.
Product Options
If you are interested in natural options for antibiotic alternatives, check out 1st Line. The 1st Line® kit has been developed as a safe and healthy alternative to an antibiotic treatment. It consists of a four-part enzymatic kit that provides 25mg of thiocyanates ions in half a litre of water. 1st Line can be used to treat all number of infections, including some of the most common, such as listeria, salmonella, streptococcus, herpes, and candida. It is also an effective staph infection treatment.
It is also worth looking at ACF228™ – Dr. Lippman’s complete antioxidant formula. This releases a blend of “free radical scavengers” in the body which support the immune system and natural defences whilst removing toxins such as heavy metals. ACF228™ contains allicin (garlic) which is a natural antibiotic alternative, alongside a multivitamin blend of Vitamins B6, B12 and folic acid.

