War on Cancer part 1 losing the war
In 1971, President Richard Nixon announced the War on Cancer and promised a cure by the 1977 bicentennial. In 2009 death rates from cancer are significantly increased and…..no cure is forthcoming! The failure of chemotherapy to control cancer has become apparent even to the oncology establishment. Scientific American featured a recent cover story entitled: “The War on Cancer — it’s Being Lost.” In it, eminent epidemiologist John C. Bailar III, MD, PhD, Chairman of the Department of Epidemiology and Biostatistics at McGill University cited the relentless increase in cancer deaths in the face of growing use of toxic chemotherapy. He concluded that scientists must look in new directions if they are ever to make progress against this unremitting killer.
Cancer incidences have grown from 1 in 500 to nearly 1 in 2 today!
Cancer remains the second leading killer in most Western industrialised nations and has crept from an incidence rate of around 1 in 500 in 1900 to 1 in 2 to 3 today. In the last 30 years there has been an 80% increase in breast cancer, a 100% increase in prostate cancer, an overall increase of 49% cancer incidence in men and 41% in women. Embodied in these facts are 2 key realities. Firstly, we are not treating cancer effectively (see below) and second, we are not preventing it!
Recently, 3 Oncologists published a key meta-analysis “The contribution of cytotoxic chemotherapy to 5-year survival in adult malignancies” in the journal Clinical Oncology (Morgan et al, 2004). Their study was based on an analysis of the results of all the randomized, controlled clinical trials (RCTs) performed in Australia and the US that reported a statistically significant increase in 5-year survival due to the use of chemotherapy in adult malignancies. Survival data were drawn from the Australian cancer registries and the US National Cancer Institute’s Surveillance Epidemiology and End Results (SEER) registry spanning the period January 1990 until January 2004. Wherever data were uncertain, the authors deliberately erred on the side of over-estimating the benefit of chemotherapy. Even so, the study concluded that overall, chemotherapy contributes just over 2 percent to improved survival in cancer patients! The authors found that the contribution of chemotherapy to 5-year survival in adults was 2.3 percent in Australia, and 2.1 percent in the USA. They emphasize that, for reasons explained in detail in the study, these figures “should be regarded as the upper limit of effectiveness” (i.e., they are an optimistic rather than a pessimistic estimate).
Why would such a key study be greeted with complete silence on this side of the world? Some practitioners still remain optimistic that cytotoxic chemotherapy will significantly improve cancer survival,” the authors wrote in their introduction. “However, despite the use of new and expensive single and combination drugs to improve response rates…there has been little impact from the use of newer regimens” (Morgan et al 2004).
At very best the worldwide success rate of chemotherapy is not more than 3%
These published statistics should not be surprising since 12 years earlier in 1992 a German epidemiologist, Dr. Ulrich Abel published a review and analysis on clinical trials of chemotherapy. He sent letters to over 350 medical centres around the world asking them to send him anything they had published on the subject. The analysis took him several years, but the results? The overall worldwide success rate of chemotherapy was only 3%. There was simply no scientific evidence available anywhere that chemotherapy can “extend in any appreciable way the lives of patients suffering from the most common organic cancers.”
To some cancer sufferers the above figures may not tally with the figures that may have been presented to prior to them prior to their chemotherapy option. The following might explain the disparity.
Oncologists frequently express the benefits of chemotherapy in terms of “relative risk” rather than giving a direct assessment of the likely impact on overall survival. Relative risk is a statistical means of expressing the benefit of receiving a medical intervention in a way that, while technically accurate, has the effect of making the intervention look considerably more beneficial than it truly is.
For example if a treatment causes a patient’s risk to drop from 4 percent to 2 percent, this can be expressed as a decrease in relative risk of 50 percent. On face value that sounds good. But another, equally valid way of expressing this is to say that it offers a 2 percent reduction in absolute risk, which is less likely to convince patients to take the treatment.
When results were expressed as a relative risk reduction, physicians believed the drugs were more effective and were strongly more inclined to prescribe than they were when the identical results were expressed as an absolute risk reduction (Bucher 1994). This is not necessarily an attempt on the Physicians part to be misleading but doctors need to be wary of the way that results are presented to them by those that have a vested interest!
The way that medical information is reported in the professional literature therefore clearly has an important influence on the treatment recommendations oncologists make. A drug that can be said, for example, to reduce cancer recurrence by 50 percent, is likely to get the attention and respect of oncologists and patients alike, even though the absolute risk may only be a small one – perhaps only 2 or 3 percent – and the reduction in absolute risk commensurately small.
Further confusion and contribution to elevated claims are the use of other surrogate end points such as ‘progression-free survival,’ ‘disease-free survival’ or ‘recurrence-free survival’ and these may only reflect temporary lulls in the progression of the disease. Such temporary stabilization of disease, if it occurs at all, seldom lasts for more than a few months at best. A correlation between shrinking a tumour and extending the life of the patient does not necessarily exist.
So, if you want to know how good a proposed chemotherapy is for you…….ask your Oncologist to tell you what is the reduction in ABSOLUTE RISK that you will achieve by having the therapy. Either, he/she will not know the answer or the true picture is likely to be not so optimistic.
The cancer industry has a turnover in excess of $200 billion annually
The reality could not be stated more clearly than by Albert Braverman, M.D., in the Lancet in 1991 “Many oncologists recommend chemotherapy for almost any type of cancer, with a faith that is unshaken by the almost constant failures”.
Putting aside for a moment the failure of science to support the widespread first line use of chemotherapy there is also the detrimental effects on quality of life that must be considered. Taken together…..we must surely, by now, have found a better way? Is a change of track not long overdue? The cancer industry turns over in excess of $200 billion annually. It is hard to believe that economics would be in the “driving seat” of this business or that this industry even remains a viable business when the outcomes are so poor. It is fear that drives most patients to accept chemotherapy together with a perhaps an unrealistic expectation of its success based on the ways that this information is conveyed to them. If we combine these ingredients with the lack of a medically-endorsed alternative treatment then we have a recipe for “Today’s cancer Therapy.”
The WHO states that at least one third of all cancer cases are preventable
As I see it there are several things that need to happen before the current tide of failure against cancer can be turned. (The following are listed in no particular order):
- Cancer therapeutics should be driven by health benefit and not by economics
- Chemotherapy should now be accepted as a failed tool in the battle and we should look away from toxic chemicals for a more effective solution. Perhaps the law around patenting of natural compound formulations needs to be re-considered.
- There are several evidence-based non-toxic therapies for cancer that have a better success in remitting cancers (some achieving 70% or more 5 year remission). I will go into more details of this in Part 2 of this article ‘winning the war on cancer.’
- Doctors should be trained in Nutritional Medicine and Preventative Medicine especially as scientific evidence accumulates in support of the gene-regulating and therefore cell-regulating role of key nutrients
- We need to detect cancer earlier. For example by the time a tumour can be seen on a mammogram it is the size of a small grape, representing 500 million cancer cells. The adjunctive use of thermal imaging would allow detection 6 to 10 years sooner (for more information see: www.chironclinic.com).
- A firm acknowledgement within the Medical fraternity that cancer is preventable. The WHO states that at least one-third of all cancer cases are preventable. Clearly they are right and if we added in the statistic of 50% reduction in risk of most cancers by correct dietary changes then we are dealing with very significant reductions in absolute risk of most cancers. Even breast cancer is only familial in approximately 8% of cases, suggesting that 92% are environmentally-caused, and by this we mean internal as well as external environment.
- Acknowledgement of and clear identification of chemicals, toxins or drugs in the external environment that increase risk with serious consideration to implementing ways to reduce them and/or exposure to them.
In the last section of this article I would like to focus briefly on the role of nutrition in cancer prevention. There are more lessons to be learned here then we may think and particularly if we still have the mindset that nutrition is just fuel for energy, growth and repair. Consider the following 2 summary statements:
- A review of 172 case-controlled prospective studies, comparing low verses high quartile of food consumption, showed that low fruit and vegetable consumption resulted in double the risk of cancer for most sites. (Block et al, Nutr Cancer Inst, 1992, 18: 1-29)
- 150 scientists reviewed 4,500 research studies on the relationship between nutrition and cancer. They found overwhelming evidence that fruits, vegetables, and grains can prevent cancer. (Cancer Prevention Research Program, 1997)
This is so important! It means that the 90% of Western populations that do not eat 5 or more portions of fruit and vegetables per day are increasing their risk of getting cancer. The risk is further compounded by addition of excess animal protein intake to this phytonutrient deficit. There is published association of animal protein intake and cancer incidence (Campbell & Campbell, 2006). This information on fruit and vegetables has led to a plethora of research on the value of anti-oxidants in cancer prevention.
What has emerged from these prospective studies is the paradoxical finding that large doses of individual anti-oxidants like Vitamin E, and beta carotene do not make any difference to cancer incidence. (Greenberg et al, 1994; Alpha-tocopherol, Beta carotene, Cancer Prevention study group, 1994; Hankinson et al, 1994; Omenn et al, 1996; Hennekens et al, 1996).
So whilst a synergy of plant-based nutrients seems to have a preventative effect, isolated anti-oxidant nutrients do not. If we look at the published scientific literature on phytonutrients we discover several important clues as to how to prevent and treat cancer. Firstly, fruit and vegetables consist of thousands of different families of nutrients e.g. Carotenoids, Flavenoids (Flavenols, Flavones, Flavenones, Isoflavones, Catechins, Anthocyanidins, Chalcones), Isoflavones (Phytoestrogens), Isothiocyanates, Organosulphur compounds, Monoterenes/Terpenoids, Resveratrolsl
As well as providing ample anti-oxidant activity these compounds have several other important published biological actions. They decrease DNA damage, improve cell communication, improve cell detoxification, are anti-inflammatory, boost Immunity, improve circulation and alter gene expression. In fact, they seem to be critically involved in the regulation of cell growth, cell cycle, apoptosis and signal transduction.
Nature is giving us the clue that cancer control requires the combination of multiple substances working in synergy
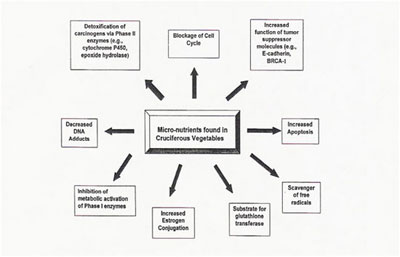
Above is a chart from the Journal of Nutrition and Cancer (2001). It shows 9 different ways that cruciferous vegetables can be anti-cancer. Six of these mechanisms involve a nutrient-gene interaction….Nutrigenomics. This has become a rapidly expanding science. It seems that phytonutrients play a key role in human gene regulation.
As cancer is essentially a cell dysregulation and plant nutrients have multiple cell regulatory actions, it becomes apparent that diets rich in these nutrients can offer protection against cancer. It is almost certain that this protective effect is NOT just based on an anti-oxidant action. Trying to fix cancer with single specific targeted compounds is not likely to be ever fruitful and yet this blinkered approach occupies almost exclusively the attention of the chemical-based Pharmaceutical Industry.
Nature is giving us the clue that cancer control requires the combination of multiple substances working in synergy but affecting cell regulation by different mechanisms. Targeting the controlling centers of cell regulation within the cell is likely to be a fruitful focus for cancer control.
References
1. Abel, U., ‘Chemotherapy of Advanced Epithelial Cancer: a critical review’, Biomedicine and Pharmacotherapy, 1992; 46: 439-452.
2. Alpha-tocopherol, Beta carotene, Cancer Prevention study group. The effect of vitamin E and beta-carotene on the incidence of lung cancer and other cancers in male smokers, N Engl J Med. 1994; 330: 1029-1035
3. Braverman,A, “Medical Oncology in the 90s”, Lancet, 1991, Vol. 337, p. 901
4. Bucher HC, Weinbacher M, Gyr K. Influence of method of reporting study results on decision of physicians to prescribe drugs to lower cholesterol concentration. BMJ. 1994;309:761-764.
5. Campbell, TC, Campbell, TM. The China Study, 2006, BenBella books
6. Greenberg, ER; Baron, JA; Tosteson, TD. A clinical trial of antioxidant vitamins to prevent colorectal adenoma, N Engl J Med. 1994;331: 141-147
7. Hankinson, SE, Stampfer, MJ. All that glitters is not beta carotene. JAMA, 1994; 272:1455-1456
8. Hennekens CH, Buring JE, Manson JE. Lack of effect of long term supplementation with beta carotene on the incidence of malignant neoplasm and cardiovascular disease, N Engl J med. 1996; 334: 1145-1149
9. Morgan G, Ward R, Barton M. The contribution of cytotoxic chemotherapy to 5-year survival in adult malignancies, Clin Oncol (R Coll Radiol), 2004;16(8):549-60.
10. Murillo, G; Mehta, RG: Cruciferous Vegetables and Cancer Prevention, Nutrition and Cancer, Volume 41, Issue 1 & 2 September 2001,17 – 28
11. Omenn GS, Goodman GE, Thornquist MD. Effects of a combination of beta carotene and vitamin A on lung cancer and cardiovascular disease, N Engl J Med. 1996; 334: 1150-1155
